Removing knotted or stuck epidural catheters: a systematic review of case reports
Article information
Abstract
Background
The knotting or in vivo entrapment of epidural catheters is an uncommon but challenging issue for anesthesiologists. This study aimed to identify the possible causes behind entrapped epidural catheters and the effective methods for their removal.
Methods
A systematic review of relevant case reports and series was conducted using the patient/population, intervention, comparison and outcome framework and keywords such as “epidural,” “catheter,” “knotting,” “stuck,” “entrapped,” and “entrapment.” The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement was followed, and the review protocol was registered with International Prospective Register for Systematic Reviews (CRD42021291266).
Results
The analysis included 59 cases with a mean depth of catheter insertion from the skin of 11.825 cm and an average duration of 8.17 h for the detection of non-functioning catheters. In 27 cases (45.8%), a radiological knot was found, with an average length of 2.59 cm from the tip. The chi-squared test revealed a significant difference between the initial and final positions of catheter insertion (P = 0.049).
Conclusions
Deep insertion was the primary cause of epidural catheter entrapment. To remove the entrapped catheters, the lateral decubitus position should be attempted first, followed by the position used during insertion. Based on these findings, recommendations for the prevention and removal of entrapped catheters have been formulated.
INTRODUCTION
Epidural anesthesia is a widely used form of regional anesthesia with a high success rate and a low complication rate. In most cases, the removal of an epidural catheter is straightforward. However, anesthesiologists occasionally face difficulties in catheter removal owing to various factors, such as the anatomy of the epidural space; diameter, tensile strength, and flexibility of the catheter; as well as the depth, level, and difficulty of its insertion. Catheters can become entangled with the nerve roots, blood vessels, lumbar fascia, posterior vertebral arches, vertebral processes, and facet joints that may pose challenges during removal. Currently, standard procedures or treatments for blocked epidural catheters are either inaccessible or rely on individual preferences and expertise.
The primary objective of this systematic review was to answer the fundamental question, “how to remove an entrapped epidural catheter?” The secondary objective was to identify the possible causes of entrapment and outcomes of entrapped catheters.
MATERIALS AND METHODS
In the absence of specific guidelines for conducting systematic review of case reports, we followed the Preferred Reporting Items for Systematic reviews and Meta‐Analyses statement, wherever applicable, for comprehensive reporting [1].
Protocol and registration
This study was registered in PROSPERO (registration number: CRD42021291266) and the International Prospective Register of Systematic Reviews.
To assess the eligibility of the research papers, we employed the PICo approach for qualitative studies, namely, Population: characteristics of the patient or population; Interest: the condition or disease of interested in; and Context: the phenomena of interest related to a defined event, activity, experience, or process.
1. Inclusion criteria
We included case reports or case series that described the insertion of an epidural catheter (population of interest), which got stuck or entrapped during removal, or in which a knot was identified after the removal or with radiological examination (the condition or disease of interested and the phenomena of interest related to a defined event, activity, experience, or process). All articles were screened to determine whether our primary question “how to remove an entrapped epidural catheter?” was addressed in this study. We limited our inclusion criteria to cases published in English before December 30, 2021.
2. Exclusion criteria
We excluded reports that did not provide an answer to the primary question, or reported the tip of the catheter to be missing after removal. Additionally, animal studies, letters to the editor, and retracted reports as well as articles without an available full text were excluded.
3. Information sources
We searched PubMed, Google Scholar, MEDLINE, and SCOPUS to find the relevant case reports or case series using keywords “epidural catheter” and one of the following terms: “knot,” “knotting,” “stuck,” “entrapped,” and “entrapment.”
Study selection process
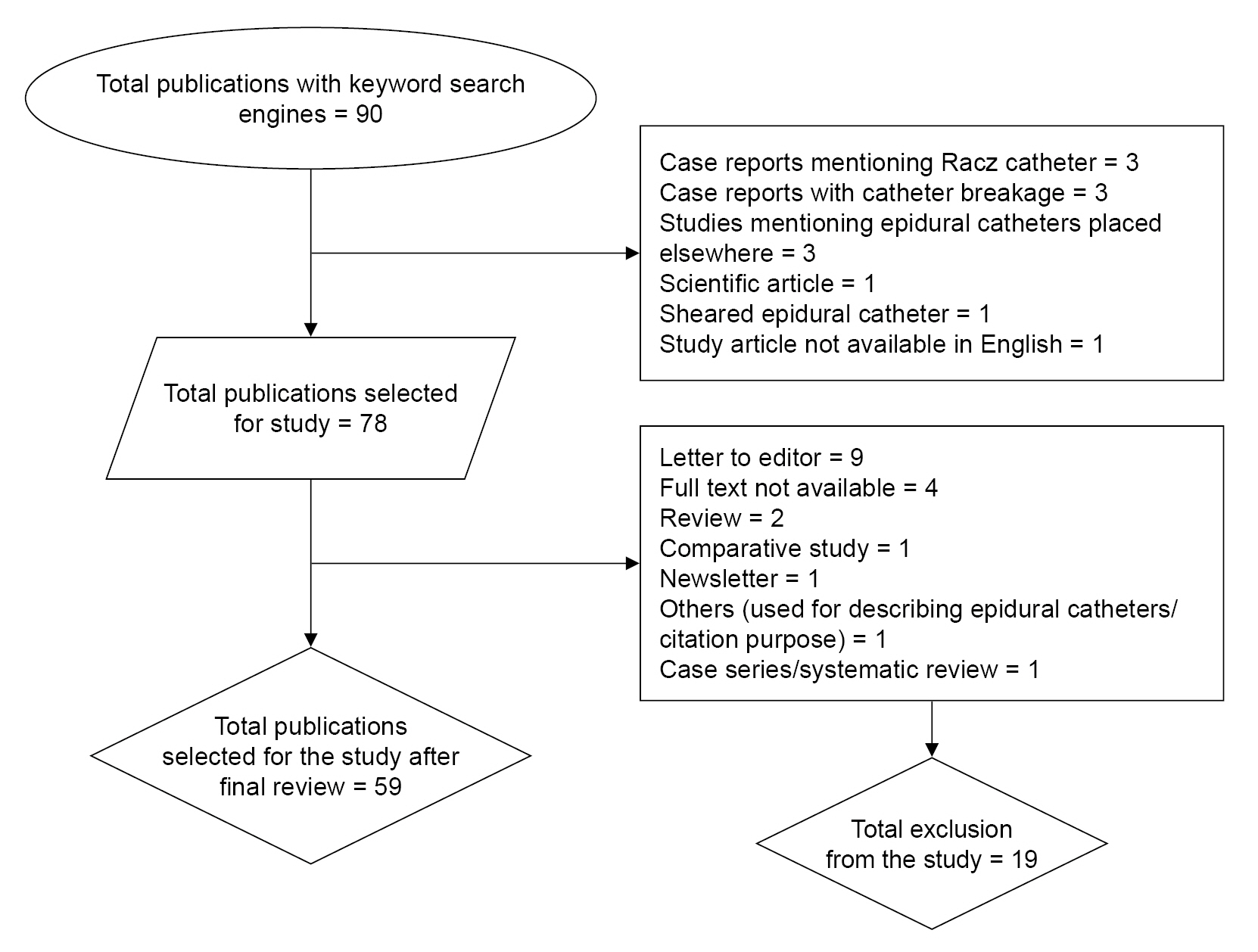
The process for selection of case reports or series has been demonstrated in Fig. 1.
Screening of the title and abstract was conducted by two authors. All reports that did not meet the inclusion criteria were excluded. Subsequently, full text reports of the selected articles were retrieved. The two authors independently examined these reports for eligibility, and additional studies were searched within the references iteratively. The list of studies was then forwarded to principal author, who developed a list of all the included and excluded articles. In the event of a disagreement between the two authors regarding the inclusion or exclusion of a report, the dispute was resolved by the principal author. The references of the selected articles were reviewed to identify any additional related articles. In case of any missing information, the corresponding authors were contacted using email addresses provided in the respective report or professional networks of researchers and scientists such as ResearchGate. In addition to seeking missing information, the authors were asked if they were aware of any other similar studies that could be included in the analysis.
1. Data collection process
After identifying the studies meeting the inclusion criteria and having the full text available, the articles were distributed to all authors for data extraction using a standardized Google Spreadsheet.
2. Data items
The extracted data included information encompassing patient characteristics (age, sex, weight, primary condition necessitating epidural placement, and patient position during insertion), any difficulties encountered during insertion, from the time of insertion (in hours) to the diagnosis of entrapment, any issues with the functionality of the catheter before knotting was detected (completely functional, partially functional, or blocked), any additional radiological studies that was conducted to confirm the diagnosis, the actions taken when a catheter was identified to be stuck, the method(s) employed for catheter removal, operator’s attributes or qualifications and years of experience, and outcome of the stuck catheter.
3. Reducing the risk of bias
We used the Risk Of Bias in Systematic Reviews (ROBIS) tool to reduce the risk of bias in methodological quality [2]. Patient/population, intervention, comparison and outcome (PICO) was employed to assess effectiveness of the reviews. One of the authors independently used the tool to evaluate the preliminary completion of manuscript writing and recommended changes, to address any perceived bias. If the source of bias could not be addressed, it was identified as a study limitation. Since all the studies were case reports, phases 2 and 3 of the ROBIS tool were not used, while phase 1 tool was used to determine the study’s relevance.
Statistical tests
Statistical analyses were performed using the SPSS software, version 23.0 (IBM Co.). For missing values of a continuous variable, we adopted a specific policy of not making any inferences when the missing values exceeded 50%, and replacing them with the average when the missing values were lower. We employed the Cohen’s kappa coefficient to measure the inter-rater agreement between two independent case study reviewers, when selecting reports to be included in the study. The Spearman’s rank correlation coefficients were used to assess correlations between variables. Categorical variables were compared using the chi-squared test. A P value of < 0.05 was considered to indicate statistical significance.
RESULTS
None of the case reports described the total number of patients in whom the epidural catheter was placed before a knot was identified, except in one patient. Therefore, the event rate and odds ratio for knotting could not be calculated. The results have been presented only in a descriptively manner in this study.
The measurement of agreement for the selection of case reports between the two reviewers using the Cohen’s kappa correlation coefficient was 0.918 for the final case selection.
Demographic characteristics
Demographic characteristics have been summarized in Table 1.

Demographic Characteristics Including Age, Sex, Weight, Indications for Epidural Placement, and Type of Epidural Catheter Used
Patient’s position during epidural insertion and the anatomical level of insertion where the catheter was placed have been described in Table 2.
We evaluated whether a specific approach, such as middle or paramedian approach, was associated with catheter entrapment. However, we found that more than 50% of this data was missing (39 cases i.e., 66.1%) having no information on the approach used. The remaining data demonstrated that 23.7% of the entrapped catheters were placed via the midline approach, whereas 10.2% were placed via the paramedian approach.
Resistance during insertion
Almost 25.4% of the cases (15 out of 59) reported that they felt resistance during insertion of the catheter or needle.
Operator’s experience
The catheter insertion was performed by anesthesiologists in seven cases (11.9%), anesthesia residents in eight cases (13.6%), and a surgeon in onecase (1.7%). The remaining 43 cases (72.9%) did not mention who performed the procedure
Depth of catheter insertion
The mean depth of catheter insertion into the skin was 11.825 cm. However, in 12 cases, the depth of catheter insertion was not mentioned. In seven cases the distance from the tip of the catheter was excluded from this depth of insertion analysis.
Functionality of the catheter
Out of 59 cases, 32 (54.2%) exhibited good functionality after insertion of the catheter before it became stuck, 3 (5.1%) had difficulty in delivering the test dose, and 13 (22.0%) had difficulty with catheter withdrawal, while functionality was not mentioned in 11 cases (18.1%). The average duration for the detection of non-functioning catheters was 8.17 hrs with an inter quartile range of 9 and a median value of 2.
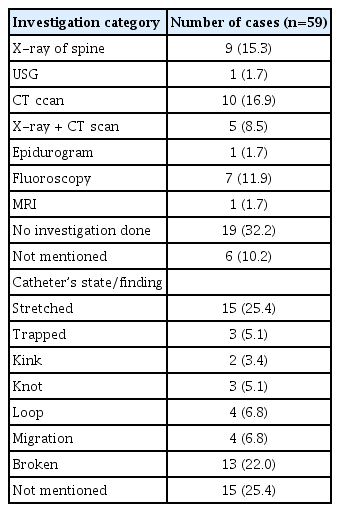
Table 3 summarizes the investigations performed for the detection of catheter entrapment and findings related to the catheter’s state.
Among the 40 case reports that were investigated, 9 of them (22.5%) failed to show the catheter position, 17 (42.5%) showed the level of catheter, 7 (17.5%) showed the level of catheter with a knot, 1 showed migration of catheter, and in 6 cases (15.0%) specific finding was not mentioned. Among the 9 cases where X-ray was the only investigation conducted, the catheter position or knot could not be revealed.
We conducted a search for positive results from radiological examinations. Among the cases examined, 27 (45.8%), exhibited the presence of a knot, 18 (30.5%) exhibited no knot, and in 14 (23.7%) cases the specific finding was not clearly mentioned. For cases with knots, the average length of the knot from the tip was 2.59 cm.
Saline flush test
A saline flush test to check the patency of the catheter was performed in only 12 cases (20.3%), and in all reported cases, the operators were unable to push the saline. In the remaining 47 cases, a saline test to check the patency of the catheter was either not performed or not mentioned.
Table 4 summarizes different methods that were used for the removal for entrapped epidural catheter and the specific recommendation for its removal.

Different Methods Implemented for Entrapped Epidural Catheter and the Specific Recommendation for Its Removal
Among the 26 cases where both position of the catheter insertion and removal was mentioned, 13 cases (22.0%) reported that the removal procedure was performed at the same position as the insertion, while 13 cases (22.0%) reported that the removal position was different from that of the insertion. A chi-squared test was performed to analyze the initial position of catheter insertion and that of the catheter removal, which showed a P value of 0.049, indicating a likelihood of the position of removal being different from that of the insertion.
Additionally, position during catheter removal was not mentioned in 20 cases (39.2%). Among the reported cases, catheter removal was performed in the prone position in 13 cases (25.5%), in lateral position in 10 cases (19.6%), and in sitting position in 7 cases (13.7%). In eight cases, the catheters were left in situ following breakage. The fate of the broken catheters over time and their follow-up findings were not mentioned in any of the studies.
DISCUSSION
Demographics of study population
The event of epidural catheter knotting and entrapment has a rate of occurrence of 0.0015% [3]. Stuck epidural catheters have been reported more commonly in middle-aged and female patients, especially during labor and delivery. Mean age of the study population was 42 years, and almost 70% of the study population was female; thus, more probability of knotted or stuck epidural was seen among the middle-aged female patients. The usage of epidural for labor analgesia or cesarean section accounted for 50% of indications for epidural administration, which led to a higher incidence of epidural-related cases among females.
Factors affecting entrapment
The position of the patient during insertion, region of the vertebral column where the catheter is inserted, and operator’s experience do not seem to influence catheter entrapment; however, an insertion length of 11 cm or more suggests a higher likelihood of entrapment, indicating that a longer insertion depth of the catheter may be associated with an increased risk.
If the distance exceeds 4.5 cm in the lumbar epidural space, the catheter is has a tendency to deviate in direction, forming a bend or loop, which may predispose it to knot formation [4]. If the catheter is inserted more than 5 cm above the level of the needle, it may curl back, leading to kinking, a turn 180° turn, and movement to opposite direction. This may result in the catheter passing out of an intervertebral foramen, wrapping around a nerve, or a combination of these complications [5]. Inserted the catheter beyond the triple mark increases likelihood for curling and knot formation, even if it is subsequently pulled back [5]. Considering the average depth of the epidural space to be 5–6 cm, the mean length of insertion of stuck catheters was approximately 12 cm; supporting the validity of the 5 cm rule [6]. Additionally, the median distance at which the knot was found was 2–3 centimeters, suggesting that not inserting a catheter beyond 5 cm from the needle tip may be the best approach to prevent possible knotting. However, many of the catheters did not have a knot, but were stretched, suggesting that other mechanisms might play a role in entrapment.
In our review, 64.4% of epidural placements were at the lumbar region, and only 5 cases reported placement above the lumbar region, which is consistent with the high incidence of obstetric cases in our study population. Most knotted catheters are inserted at the lumbar level, especially in obstetric patients, and a knot is formed along the last 3 cm of the catheter [7]. Muneyuki et al. [8] reported that an indwelling thoracic epidural catheter was less likely to curl, bend, or kink in the epidural space than an indwelling lumbar epidural catheter, and a greater amount of the catheter could be inserted without coiling, which attributes to the difference in the angle of insertion of the needle. In the lumbar region, the epidural needle impinges on the dura at a right angle, whereas in the thoracic region, the needle is inserted at an obtuse angle to the epidural canal, making it easier to insert the catheter straight [9]. Nevertheless, the exact rates of stuck epidural catheters in the thoracic and lumbar regions could not be determined in this study.
Tunneling the epidural catheter by 5 cm in a cohort of 82 patients was associated with reduced catheter motion; however, the percentage of catheters maintaining the original position was not statistically different [10]. Nevertheless, it is important to note that our study did not evaluate whether tunneling reduces the possibility of knot formation as this has not been consistently reported in the included studies.
Knot formation
The mean position of knot formation in our study was 2.59 cm from the tip, which is consistent with the findings of a study by Lim et al. [11] In their study, 13% of lumbar catheters inserted in a group of 45 males were advanced more than 4 cm without coiling, and coiling occurred at a median length of 2.8 cm from the catheter tip [11]. Based on 18 case reports, the frequency of knotted catheters is estimated to be 1:2000–30,000 epidurals, with 87% of the knots occurring < 3 cm from the catheter tip and 28% of the knots associated with a loop in the catheter [12], which is consistent with our study findings.
In cadavers study using epiduroscopy, paramedian catheters were observed to cause less epidural tenting and pass cephalad more reliably than midline catheters [13]. In our study, we observed that 66.1% of data (39 cases) were missing regarding approach used for epidural catheter placement. Among the available data, 14 cases (23.7%). had catheter placement in the midline, and 6 cases (10.2%) underwent the paramedian approach. Since only a few cases underwent the paramedian approach, it is possible that less tenting or knots were observed with this approach. However, it is evident from our review that a knot formation during or after a paramedian insertion approach is not uncommon.
Techniques for catheter removal
A total of 47.5% cases underwent catheter removal with traction. Among them 13.6% had the catheter removed in the same position as that of insertion, whereas 8.5% had it removed in a different position. These findings align with the recommendation put forward by Morris et al. [14], which suggests that whenever the removal of catheter becomes difficult, the recommendation is to pull out softly and steadily, with the patient in the same position as that during catheter insertion; if this approach fails, an alternative strategy is to attempt catheter removal with the patient placed in different positions and at various angles of lumbar flexion or extension. Another method, traction was recommended by Lala et al. [15], who suggested that steady traction would allow the catheter and knot to decrease in diameter and facilitate easy passage through ligaments.
Consistent with our study findings, previous studies have suggested that removal is the easiest if the patient is in the same position as that during insertion [16]. This observation is in line with a report by Morris et al. [14], where they found that significantly less force was required when the patient was placed in the same position for withdrawal as that for insertion.
Among the cases in which the catheter was removed, 13 reported removal in a prone position (25.5%), 10 (19.6%) in lateral, and only 7 (13.7%) in sitting position. Cases that reported removal in the prone position were performed under anesthesia, whereas the lateral position was most successful for catheter removal without anesthesia. We presume that all cases in which successful removal occurred in the prone position were probably planned for surgical removal and were kept in that position after administration of general anesthesia; however, the specific contribution of the prone position and general anesthesia in facilitating successful removal is unclear. The sitting position places more force on the spine, creating increased resistance to withdrawal. The force required to remove a lumbar catheter was 2.5 times more in the sitting position than that in the lateral position [17]. Blackshear et al. [18] suggested that less tension is required to remove the catheter when the patient is in the lateral decubitus position as opposed to the sitting position. According to Boey and Carrie, lateral positioning allowed a 2.5 N reduction in the force needed to withdraw the epidural catheter in the median and paramedian approaches [19].
Catheter characteristics
Arrow brand catheters (Arrow, USA) have been reported to stretch more than other catheter brands (Perifix, B Braun; Perisafe, Becton, Dickinson and Co., Portex) and break at lower forces than other brands of epidural catheters, especially at the 5 cm mark [20]. Our study findings did not show significant differences between the catheter brands used for knot formation. A study by Blum and Sosis showed that Abbott epidural catheters (nylon, Abbott Laboratories Inc.) were significantly stronger, whereas Baxter catheters (nylon, Baxter Healthcare Co.) were the weakest among the six different types of commercially available 20 G epidural catheters [21]. Spring wire-reinforced catheters are more resistant to kinking and more patent. An unconstrained tug on any epidural catheter (polyamide, polyurethane, or fluorinated ethylene propylene) should not be attempted as it could conceivably be around a nerve root or result in a piece of any manufacturer’s catheter breaking off [22]. Applying traction to the catheter resulted in its breakage in approximately 30% of cases [10]. The incidence of catheter breakage was not assessed in our study because patients with broken catheters were excluded.
During difficult catheter removal, normal saline can be injected through the catheter before making another removal attempt [23]. Injection of sterile saline and rotation of catheter was unsuccessful in catheter withdrawal as demonstrated in a study by Brenier et al. [24]. Our study reported similar findings, as all 12 cases (20.3%) in which a saline flush test was performed were unsuccessful. An unsuccessful saline flush test indicates the presence of a knotted catheter.
Investigations for entrapped catheters
In 32.2% of the case reports, no investigations were carried out, whereas 10.2% cases it was not specified if any investigation was done. Among the nine cases in which lumbosacral spine radiography was performed, five failed to reveal the catheter position or knot. A similar suggestion was made in a study by Asai et al. [20], in which even radiopaque catheters could not be visualized on a radiograph of the spine, especially when they were located in the epidural space. Fluoroscopy was done in only 11.9% of cases. If the epidural catheter is radio-opaque and patent, fluoroscopic examination with contrast may be useful, although they are not always successful. A total of 25.4% patients had undergone computed tomography (CT) scans to detect knot/catheter position with positive results. CT scans have been recommended for locating retained catheters because of their high resolution and ease of testing [25]. Two case reports by Bréget et al. [26] successfully visualized the epidural knot/loop on CT scans. CT scans may be helpful in identifying knots. However, it is important to note that not all entrapped catheters have a knot, as they may be stretched without forming a knot.
Breakage, hematoma formation, epidural site infection, and neurological deficits are common complications of catheter entrapment. However, we did not study the complications associated with catheter entrapment, or some of the included studies did not report any complications.
Outcomes and removal of entrapped catheters
In our study, 18 cases (30.5%) underwent surgical removal, of which 25.4% were done under general anesthesia and 5.1% were under local anesthesia. It is important to note that 17 case reports (28.8%) recommended some form of traction for the removal of catheters. Surgical removal was recommended only in six case reports (10.2%). Surgical removal of a broken catheter is not mandatory if the patient remains asymptomatic [10]. It is reasonable to surgically remove the epidural catheter in children to reduce the possibility of neurological problems through growth and development or in adults with definite neurological symptoms, as well as in cases in which the catheter tip is in the dura [23]. During catheter removal, it is important to ensure that patients should not experience pain, which may indicate the possibility of the cathetert being tangled around the nerve root. Owing to the possibility of nerve root avulsion, the catheter should be removed under direct visualization via laminectomy [17]. Five case studies (8.5%) recommended leaving the catheter in situ if no complications were observed.
Recommendations
1) To prevent knotting and entrapment, the length of the inserted catheter should be limited to less than 5 cm. A catheter with a greater tensile strength should be chosen.
2) If catheter entrapment is suspected, the saline flush test should be carried out to check the functionality. If the test fails, there is a high risk of catheter knotting.
3) What types of investigations should be conducted? Lumbosacral CT scan should be the investigation of choice, as radiography of the lumbosacral spine may not identify the knot. Radiological investigation is not always required.
4) A common method of removal is gentle traction on the catheter; thus, traction application should be the first choice.
5) Removal of the knotted epidural catheter in the lateral position should be attempted first. If this fails, a second attempt should be performed in the same position as that of the insertion. Avoid undue force during the removal process to minimize the risk of complications or further entanglement.
6) If the second attempt fails and the patient has neurological symptoms, surgical removal under Local anesthesia, Regional anesthesia, and/or General anesthesia should be considered.
7) Catheter removal by gentle traction can be performed by placing the patient in the prone position during surgical removal.
8) Following catheter breakage, if the patient is asymptomatic, the catheter can be left in situ after providing necessary counseling.
Limitations
This systematic review was unable to deliver quantitative data. It was not possible to prove a cause-and-effect relationship or allow generalizations. Furthermore, there is a risk of over-interpretation and publication bias as only cases with successful catheter removal may have been published. With the availability of comprehensive national-level data in some countries, this review will help to design new studies that may address such biases.
Conclusion
Our study highlights the potential for catheter entrapment in the epidural space, with deeper insertions significantly contributing to knotting and entrapment. When faced with an entrapped catheter, the initial attempt at removal should be in the lateral decubitus position, followed by the position used during insertion. CT scan may prove beneficial in identifying the presence of a knot.
Furthermore, our findings suggest that factors beyond deeper insertion and knotting may contribute to catheter entrapment, as evidenced by the instances of catheter stretching during challenging removal. In cases where the epidural catheter breaks during removal, the catheter may be left in situ under close monitoring in asymptomatic patients.
The results of this study have implications for clinical practice, emphasizing the importance of careful catheter insertion and management techniques. Further research is warranted to better understand the underlying factors contributing to epidural catheter entrapment and develop more effective preventive strategies.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
All data generated or analyzed during this study are included in this published article.
AUTHOR CONTRIBUTIONS
Conceptualization: Bikash Khadka, A Sharma.
Data curation: Bikash Khadka, Ashim Regmi, Anup Ghimire.
Formal analysis: Bikash Khadka, A Sharma, Anup Ghimire, Prajjwal Raj Bhattarai.
Funding acquisition: Anup Ghimire.
Methodology: Bikash Khadka, Ashim Regmi.
Project administration: Bikash Khadka, A Sharma, Anup Ghimire, Prajjwal Raj Bhattarai.
Writing - original draft: Bikash Khadka.
Writing - review & editing: Bikash Khadka, Ashim Regmi, Anup Ghimire, Prajjwal Raj Bhattarai.
Investigation: Bikash Khadka, Ashim Regmi, Prajjwal Raj Bhattarai.
Resources: Anup Ghimire, Prajjwal Raj Bhattarai.
Software: Ashim Regmi. Supervision: A Sharma, Prajjwal Raj Bhattarai.
Validation: A Sharma.