|
 |
- Search
| Anesth Pain Med > Volume 18(3); 2023 > Article |
|
Abstract
Background
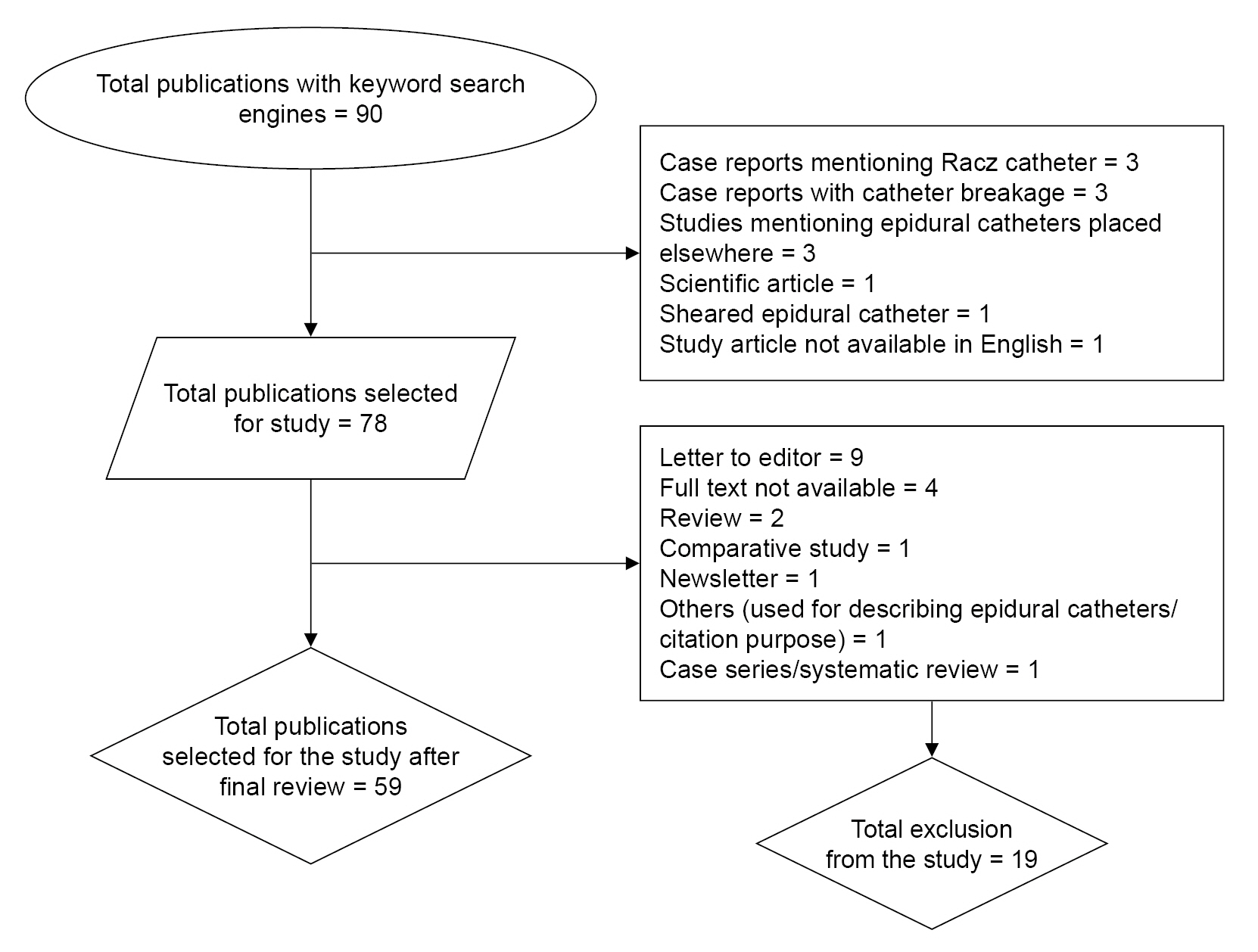
Methods
Results
Conclusions
Notes
DATA AVAILABILITY STATEMENT
All data generated or analyzed during this study are included in this published article.
AUTHOR CONTRIBUTIONS
Conceptualization: Bikash Khadka, A Sharma.
Data curation: Bikash Khadka, Ashim Regmi, Anup Ghimire.
Formal analysis: Bikash Khadka, A Sharma, Anup Ghimire, Prajjwal Raj Bhattarai.
Funding acquisition: Anup Ghimire.
Methodology: Bikash Khadka, Ashim Regmi.
Project administration: Bikash Khadka, A Sharma, Anup Ghimire, Prajjwal Raj Bhattarai.
Writing - original draft: Bikash Khadka.
Writing - review & editing: Bikash Khadka, Ashim Regmi, Anup Ghimire, Prajjwal Raj Bhattarai.
Investigation: Bikash Khadka, Ashim Regmi, Prajjwal Raj Bhattarai.
Resources: Anup Ghimire, Prajjwal Raj Bhattarai.
Software: Ashim Regmi. Supervision: A Sharma, Prajjwal Raj Bhattarai.
Validation: A Sharma.
Table┬Ā1.
Table┬Ā2.
Table┬Ā3.
Table┬Ā4.
REFERENCES
-
METRICS

-
- 0 Crossref
- 2,833 View
- 83 Download
- Related articles in Anesth Pain Med
-
Real-time ultrasound guided thoracic epidural catheterization: a technical review 2021 October;16(4)
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others