 |
 |
- Search
| Anesth Pain Med > Volume 15(2); 2020 > Article |
|
Abstract
Background
Although systolic anterior motion (SAM) of the mitral valve anterior leaflet is well-known to cause hemodynamic perturbation in many anesthetic situations, the prevalence and clinical implication of SAM of mitral chordae tendineae (chordal SAM) in liver transplantation (LT) has not been evaluated. We aimed to assess the impact of chordal SAM on intraoperative postreperfusion syndrome and short and long-term all-cause mortality.
Methods
We retrospectively evaluated 1751 LT recipients from January 2011 to June 2017 who had preoperative echocardiography. Echocardiography-derived parameters and the prevalence of post-reperfusion syndrome between those with chordal SAM and without chordal SAM were compared. The cumulative mortality rate according to the presence of chordal SAM was evaluated by the Kaplan-Meier survival curve.
Results
Of the enrolled recipients, 21 (1.2%) had chordal SAM in preoperative echocardiography. Compared to those without chordal SAM, patients with chordal SAM had a smaller end-systolic volume index (median 18 ml/m2 vs. 22 ml/m2, P = 0.015) and end-diastolic volume index (median 52 ml/m2 vs. 63 ml/m2, P = 0.011). However, there was no difference in systolic and diastolic function in echocardiography. The prevalence of intraoperative post-reperfusion syndrome did not show any difference (42.9% vs. 45.3%, P = 1.000). Over the mean 4.8-year follow-up, cumulative 90-day and overall mortality also did not show a difference (Log rank P > 0.05, both).
Systolic anterior motion (SAM) of the mitral chordae tendineae (chordal SAM) is commonly observed with septal hypertrophy in hypertrophic cardiomyopathy (HCM) and may cause severe hypotension by obstructing the left ventricular outflow tract (LVOT) during the systole phase. However, various patterns of SAM are known to occur even in cases other than HCM [1]. This disease has drawn the attention of anesthesiologists due to the fact that SAM causes an obstruction of the LVOT during anesthesia and induces severe hemodynamic instability that may be low-responsive to the conventional treatment [2].
In chordal SAM, the chordae tendineae moves anteriorly during the systolic phase and is known to be associated with mitral valve prolapse [3]. It is a rare endocardial change with a prevalence of 3.9% among patients with mitral valve prolapse and 1% among the normal population [3]. However, its hemodynamic impact during anesthesia or effects on postoperative clinical outcomes are unknown.
We hypothesized that the incidence of chordal SAM might be higher among patients with end-stage liver disease who have hyperdynamic circulation compared to that among the general population. Moreover, we also hypothesized that patients with chordal SAM will be more vulnerable to postreperfusion syndrome because of increased hyperdynamic circulation due to a sudden drop in systemic vascular resistance during graft reperfusion and the use of cardiovascular drugs like epinephrine could induce a structural change of the heart.
Therefore, this study aims to examine the prevalence of chordal SAM in echocardiography before liver transplantation (LT), characteristics of patients with chordal SAM, and the effects of chordal SAM on reperfusion syndrome during LT, postoperative mortality, and liver failure.
This observational study was approved by the Institutional Review Board at the Asan Medical Center (no. 2019-0174), and patients with end-stage liver disease who underwent LT at our hospital between January 2011 and June 2017 were retrospectively reviewed. Patients under the age of 18, patients undergoing a re-transplantation, patients who did not undergo echocardiography preoperatively, patients with chronic kidney disease, and patients with missing data were excluded. At our hospital, all LT patients undergo transthoracic echocardiography. In this study, we collected information about patients’ state, including transthoracic echocardiography results, and laboratory test results from electronic medical records and retrospectively analyzed them. Transthoracic echocardiography (Hewlett-Packard Sonos 2500 or 5500 imaging system, Hewlett-Packard Inc., USA) was performed by a skilled echocardiography technician using a 2.5 MHz transducer and the results were confirmed by an attending cardiologist. The incidence of reperfusion syndrome and the epinephrine dose during the reperfusion period was collected. The 90-day mortality as well as overall mortality and graft failure during the entire period of observation were assessed. Postreperfusion syndrome was defined as a more than 30% drop of the mean arterial pressure from the baseline that persists for at least one minute during the first five minutes after reperfusion of the transplanted liver. Time until graft failure was defined as death after transplantation or re-transplantation, whichever came earlier. Information about the patient’s death was collected from our LT patient list and electronic medical records. The mean observation period was 4.8 ± 2.0 years, with a mean period of 4.3 ± 2.4 years for patients with SAM and 4.8 ± 2.0 years for those without SAM.
Continuous variables were described as mean ± SD or median (1Q, 3Q), and categorical variables were described as the number of patients and percentage. Continuous variables were analyzed with the Shapiro Wilk normality test followed by the Student’s t-test or Mann-Whitney test, while categorical variables were analyzed with either the chi-square test or Fisher's exact test. The differences in mortality rates between the two groups were analyzed using the Kaplan-Meier survival curve and log-rank test. The “moonBook” [4] and “survival” [5] R package were used for statistical analyses. Statistical analyses were performed using R (version 3.3.1, R foundation for statistical Computing, Austria). A P value < 0.05 was considered statistically significant.
Of the LT patients between January 2011 and June 2017, a total of 1,751 patients was enrolled after the exclusion and 21 (1.2%) showed chordal SAM. The representative manifestation of chordal SAM is presented in Fig. 1 and Supplementary Video 1. Table 1 shows the patients’ demographics and cause of liver cirrhosis according to chordal SAM. There were no differences in the age, sex, Model for End-Stage Liver Disease score, and the prevalence of underlying diseases such as hypertension and diabetes mellitus between the two groups. Table 2 shows the results of echocardiography between the two groups.
There was no difference in the grade of mitral regurgitation (P = 0.815) or in left ventricular systolic and diastolic functions between the two groups (Table 2). However, regarding heart volume, patients with chordal SAM had a smaller end-systolic volume index (median 18 [15, 25] ml/m2 vs. 22 [19, 27] ml/m2, P = 0.015) and end-diastolic volume index (median 52 [42, 68] ml/m2 vs. 63 [54, 74] ml/m2, P = 0.011) compared to that of patients without chordal SAM.
Table 3 shows a comparison of intraoperative hemodynamic changes (presence of postreperfusion syndrome) and the epinephrine dose used as well as 90-day mortality, overall mortality, 90-day graft failure, and overall graft failure after LT. There were no differences in the incidence of intraoperative reperfusion syndrome (42.9% vs. 45.3%, P = 1.000) and the epinephrine dose used (P = 0.925) between the two groups. Further, the two groups also did not differ in the 90-day mortality (4.8% vs. 2.6%, P = 1.000), overall mortality (9.5% vs. 10.6%, P = 1.000), 90-day graft failure (4.8% vs. 3.1%, P = 1.000), and overall graft failure (9.5% vs. 12.3%, P = 0.964) (Fig. 2). There were also no differences in cumulative 90-day and overall mortality (Log-rank P for 90-day mortality = 0.548; Log-rank P for overall mortality = 0.900) according to the presence of chordal SAM (Fig. 3).
The prevalence of chordal SAM discovered in the preoperative echocardiography was 1.2%, and patients who had chordal SAM did not significantly differ in the incidence of postreperfusion syndrome during LT from patients who did not have chordal SAM. Moreover, the two groups of patients did not significantly differ in the 90-day mortality and overall mortality during the observation period.
End-stage liver disease is known to cause cardiac structural impairments and dysfunctions, such as tachycardia, systolic and/or diastolic functions, and/or electrophysiology, which is defined as cirrhotic cardiomyopathy (CCMP) [6]. Structural changes of the heart generally involve left ventricular enlargement and hypertrophy and cardiac tissues show myocardial fibrosis and subendocardial edema. Further, the increase of heart rate in response to beta receptor agonists, such as isoproterenol, is diminished in patients with liver cirrhosis, as seen in in rat models [7]. Although the systolic functions and cardiac output are generally normal or elevated during rest, patients with CCMP have been reported to show reduced cardiac systolic function during stress situations, such as exercise and bleeding [8-11]. Moreover, diastolic dysfunction frequently occurs, and particularly, preoperative diastolic disorder is closely related to increased postoperative mortality following LT [12].
In our study, a comparison of clinical features between patients with and without chordal SAM revealed that patients with chordal SAM had a smaller left ventricle (LV) dimension in systole (28 vs. 30, P = 0.048). Considering that LV dimension in systole is an indicator of cardiac systolic function, this result suggests that chordal SAM occurred in patients with a small heart (low end-diastolic volume index) with greater hyperdynamic circulation. However, the two groups did not significantly differ in other systolic indices, such as ejection fraction, therefore further research is needed regarding the relationship between chordal SAM and hyperdynamic circulation. Furthermore, additional studies are needed to identify the clinical implications of such differences. In addition, whereas previous studies reported that chordal SAM is more common among patients with mitral valve prolapse syndrome, no significant difference was found in our study. The reason behind this should also be studied on a larger study population [3].
SAM is a phenomenon in which the anterior motion of the anterior mitral leaflet causes an obstruction of the LVOT, and eventually, a severe cardiovascular collapse. Although SAM is commonly known to be induced by myocardial thickening and asymmetrical interventricular septal thickening, it can be caused by severe hypovolemia, use of dobutamine, and/or elevated catecholamine secretion caused by stress even in patients without anatomical defects, necessitating close attention. Particularly, LT can cause severe hypovolemia due to ligation of the inferior vena cava and massive bleeding during surgery. Therefore SAM can occur in patients with CCMP, ischemic heart disease, or hepatorenal syndrome who develop a postreperfusion syndrome because high doses of cardiovascular drugs are used in such cases. Therefore, it is standard protocol to suspect SAM as a cause of unexplained severe hypovolemia during LT, and numerous relevant case studies have been reported [13-15]. We hypothesized that chordal SAM, though not the typical SAM of the anterior mitral leaflet, may have some impact on reperfusion syndrome. However, our results showed no significant differences. Moreover, there were no significant differences in the postoperative 90-day and long-term mortality after LT.
One limitation of this study is that although we examined a relatively large number of LT patients, our specific study population was small, as chordal SAM is a rare disease. Subsequent studies should recruit a larger study population. Further, as this study is a retrospective analysis, we could not include the use of echocardiography upon the onset of postreperfusion syndrome. Even if the incidence of postreperfusion syndrome may not differ, the onset of SAM that causes hemodynamic changes can be observed, so subsequent studies should utilize echocardiography during LT.
In conclusion, chordal SAM was found in 1.2% of patients before LT, and these patients had smaller cardiac systolic and diastolic volumes than those without chordal SAM. Unlike with the SAM of the anterior mitral leaflet, the incidence of intraoperative postreperfusion syndrome or postoperative 90-day and overall mortality did not significantly differ according to chordal SAM. Therefore, it seems safe for patients with chordal SAM to undergo LT, but more prospective studies with echocardiography data during postreperfusion period are needed.
SUPPLEMENTARY MATERIALS
Supplementary data including video 1 and Korean version of this article are available at https://doi.org/10.17085/apm.2020.15.2.187
Fig. 1.
Representative figure of echocardiographic finding of chordae systolic anterior motion of mitral valve in parasternal long axis view.
Arrow represents the systolic motion of mitral valve.
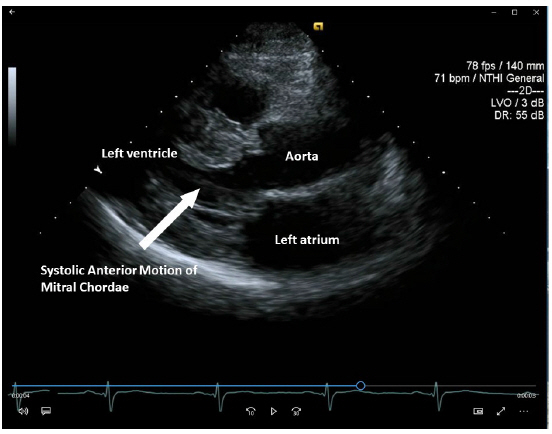
Fig. 2.
Comparison of rate of 90-day (A) and overall mortality (B) between patients with or without chordae systolic anterior motion of the mitral valve. SAM: systolic anterior motion of mitral valve.
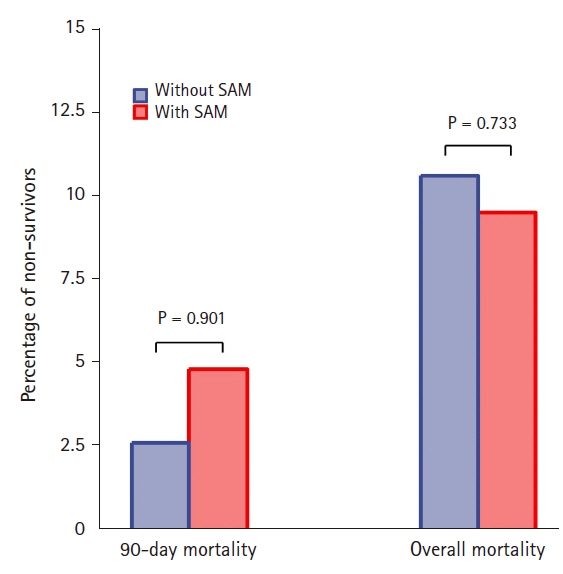
Fig. 3.
Cumulative 90-day (A) and overall mortality (B) compared between the groups of patients with or without chordae systolic anterior motion of mitral valve. No difference was found between the patients. SAM: systolic anterior motion of mitral valve.

Table 1.
Demographic of Liver Transplant Recipients according to Prevalence of Chordal Systolic Anterior Motion (SAM) of Mitral Value
Table 2.
Echocardiography of Liver Transplant Recipients according to Prevalence of Chordal Systolic Anterior Motion (SAM) of Mitral Value
Table 3.
Intraoperative Hemodynamic Changes and Outcomes after Post-liver Transplantation
| Variables | Without chordal SAM (n = 1,730) | Chordal SAM (n = 21) | Total (n = 1,751) | P value |
|---|---|---|---|---|
| Intraoperative pRBC transfusion | 7 (2, 14) | 5.0 (0, 14) | 7 (2, 14) | 0.425 |
| Post-reperfusion syndrome | 783 (45.3) | 9 (42.9) | 792 (45.2) | 1.000 |
| Epinephrine dose (µg)* | 0 (0, 10) | 0 (0, 10) | 0 (0, 10) | 0.925 |
| 90-day mortality | 45 (2.6) | 1 (4.8) | 46 (2.6) | 1.000 |
| Overall mortality | 184 (10.6) | 2 (9.5) | 186 (10.6) | 1.000 |
| 90-day graft failure | 54 (3.1) | 1 (4.8) | 55 (3.1) | 1.000 |
| Overall graft failure | 212 (12.3) | 2 (9.5) | 214 (12.2) | 0.964 |
REFERENCES
1. Manabe S, Kasegawa H, Arai H, Takanashi S. Management of systolic anterior motion of the mitral valve: a mechanism-based approach. Gen Thorac Cardiovasc Surg 2018; 66: 379-89.



2. Moon YJ, Park JH, Oh J, Lee S, Hwang GS. Harmful effect of epinephrine on postreperfusion syndrome in an elderly liver transplantation recipient with sigmoid ventricular septum: a case report. Medicine (Baltimore) 2016; 95: e4394.



3. Pearson AC, Pasierski TJ, Orsinelli DA, Gray P, Huschart K. Systolic anterior motion of the mitral chordae tendineae: prevalence and clinical and Doppler-echocardiographic features. Am Heart J 1996; 131: 748-53.


4. Moon KW. R statistics and graphs for medical papers. Seoul, Hannaare. 2015.
5. Therneau TM. A Package for survival analysis in S. R package version 2.37-7. 2014 [cited 2019 Apr 27]. Available from: http://CRAN.R-project.org/package=survival.
6. Kwon HM, Hwang GS. Cardiovascular dysfunction and liver transplantation. Korean J Anesthesiol 2018; 71: 85-91.




7. Ramond MJ, Comoy E, Lebrec D. Alterations in isoprenaline sensitivity in patients with cirrhosis: evidence of abnormality of the sympathetic nervous activity. Br J Clin Pharmacol 1986; 21: 191-6.



9. Wong F, Girgrah N, Graba J, Allidina Y, Liu P, Blendis L. The cardiac response to exercise in cirrhosis. Gut 2001; 49: 268-75.



10. Møller S, Henriksen JH. Cirrhotic cardiomyopathy: a pathophysiological review of circulatory dysfunction in liver disease. Heart 2002; 87: 9-15.



12. Mittal C, Qureshi W, Singla S, Ahmad U, Huang MA. Pre-transplant left ventricular diastolic dysfunction is associated with post transplant acute graft rejection and graft failure. Dig Dis Sci 2014; 59: 674-80.



13. Harley ID, Jones EF, Liu G, McCall PR, McNicol PL. Orthotopic liver transplantation in two patients with hypertrophic obstructive cardiomyopathy. Br J Anaesth 1996; 77: 675-7.



- TOOLS
-
METRICS

-
- 1 Crossref
- 6,783 View
- 144 Download
- Related articles in Anesth Pain Med
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others







