INTRODUCTION
When acute postoperative pain is insufficiently controlled, the pain can induce emergence agitation after general anesthesia and affect the recovery of the patient after surgery. Uncontrolled pain can be a leading cause of delayed discharge, and can transition to chronic pain. Proper selection of analgesics during the acute postoperative stage is critical. Opioid analgesics offer more effective pain relief without ceiling effects and are commonly used for treating postoperative pain [
1,
2]. Fentanyl has an acute onset of action and a shorter action duration compared with other opioids, and is therefore frequently used for moderate to severe postoperative pain. Clinical experience of analgesia with oxycodone has also gradually increased after its approval by the Ministry of Food and Drug Safety of Korea. Oxycodone is a strong opioid with a longer duration of analgesia than that of fentanyl, and provides effective analgesia in cases of acute postoperative pain [
3].
To choose an adequate opioid dosage, clinicians must understand the pharmacological profile of each opioid drug. The safe dose margin of oxycodone and the direct conversion factor between intravenous (IV) oxycodone and IV fentanyl has not yet been established. Oxycodone also causes opioid-related side effects, such as nausea, vomiting, pruritus, constipation, respiratory depression, and sedation; therefore, further studies of oxycodone are needed to titrate the dose according to the intensity of stimulation in various type of pain. Before oxycodone can become the treatment of choice for postoperative pain relief, the substantial limitations to its use need to be addressed.
No previous study has compared the effect of an IV bolus of oxycodone and fentanyl in dental surgery. Therefore, we prospectively compared the analgesic efficacy of oxycodone to that of fentanyl, which is mainly used to treat acute moderate to severe postoperative pain after cyst enucleation with surgical extraction of impacted teeth, and aimed to examine the related adverse events.
MATERIALS AND METHODS
This randomized, double-blind, clinical trial was approved by the Institutional Review Board of Kyungpook National University Hospital, and all patients signed written informed consent. All patients, aged 16 to 68 years, who underwent cyst enucleation with surgical extraction of impacted teeth under general anesthesia, from November 2016 to May 2017 in our hospital, were enrolled. The primary exclusion criteria were allergic reactions to morphine or fentanyl; a history of regular use of opioids, other analgesics, sedative medication, or corticosteroids; pregnancy; underlying hepatic, renal, pulmonary, or cardiac disease; difficult intubation or risk of aspiration pneumonia; and active upper respiratory tract infection. On the day before surgery, the study procedure was explained to the patients once again.
No patients received premedication. General anesthesia was induced with 2 mg/kg propofol and 0.6 mg/kg rocuronium, and naso-tracheal intubation was performed. The patients were ventilated with a mixture of 50% nitrous oxide in oxygen, and anesthesia was maintained by desflurane. In the operating room, patients were monitored by means of pulse oximetry, electrocardiography, Bispectral Index (BIS), and non-invasive blood pressure measurements taken at 5-minute intervals. The pressure of the endotracheal tube balloon cuff was maintained under 25 mmHg. Mechanical ventilation was performed with a tidal volume of 8-10 ml/kg and a respiratory rate of 8-15 breaths/min, with the aim of maintaining the partial pressure of end-tidal carbon dioxide at 30-40 mmHg. Anesthesia was maintained with desflurane (6-9 vol%), to maintain a BIS between 40 and 60. Blood pressure and heart rate were maintained within 20% of the pre-anesthetic values. No additional injection of neuromuscular blocking agent was given. Neuromuscular blockade was reversed with 0.2 mg/kg pyridostigmine and 0.01 mg/kg glycopyrrolate, and reversal was confirmed by more than 90% response of train-of-four monitoring on the ulnar nerve. Tracheal extubation was performed when patients obeyed verbal commands and spontaneous respiration was restored.
Patients in both groups were randomly divided into an oxycodone group (Group O, 0.05 mg/kg, n = 36) and a fentanyl group (Group F, 1 μg/kg, n = 36) using Excel 2013 (Microsoft Corp., USA). The analgesic solution was prepared in a syringe as either 1 mg/ml oxycodone or 5 μg/ml fentanyl, made up to 20 ml with 0.9% saline, according to the randomization sheet. The doctor who prepared the syringes did not participate in the patients’ anesthesia or recovery process. The allocated syringe was then presented to another anesthetist, who was also not involved in the study, for administration. Neither the anesthetist nor the assessor in the post-anesthetic care unit (PACU) was aware of which solution the patient was administered. These injections were administered 10 minutes before completing the final suture. For suppression of potential postoperative nausea and vomiting (PONV), all patients received 0.075 mg IV palonosetron after induction of general anesthesia.
In a pilot study, with a potency ratio of 60:1 (oxycodone: fentanyl), with reference to the results of Park et al. [
4], we found that the analgesic effect of oxycodone was excellent. However, the recovery time was significantly longer than that of fentanyl, and four of seven patients who had received oxycodone experienced moderate to severe PONV. Thus, we modified the potency ratio to 50:1 for this study.
The duration of anesthesia (from induction to tracheal extubation) was recorded, as was the duration of surgery, which was taken as the time from the first incision to the final stitch. The recovery time (from the cessation of administration of nitrous oxide and desflurane to tracheal extubation) was also recorded. After emergence from anesthesia, all the patients remained in the PACU for 1 hour. The following parameters were assessed at 15, 30, and 60 minutes, and 6 hours after arrival in the PACU: noninvasive blood pressure, heart rate, visual analogue scale (VAS) score for pain, PONV (verbal rating scale; mild, moderate, and severe nausea), Pasero opioid-induced sedation scale (S, asleep but easily roused; 1, awake and alert; 2, occasionally drowsy, easily roused; 3, frequently drowsy, falls asleep during conversation; 4, somnolent, minimal or no response to stimulation), headache, dizziness, sore throat, and side effects of opioid analgesics (pruritus, respiratory depression, etc.). In patients with moderate pain, based on a VAS score of 4 or more in the PACU, rescue analgesics (IV fentanyl 0.5 μg/kg) were administered. The patient’s pain was monitored in the PACU, and if the patient required additional analgesics, rescue analgesic was administered at the same dose. The time of first demand for rescue analgesic in the PACU was also recorded. In the PACU, when a patient complained of a moderate or severe grade of nausea and vomiting, 0.3 mg IV ramosetron was administered. Before discharge from the hospital, patients were questioned about their overall satisfaction with the postoperative analgesia treatment, using a 5-point scale (1, very unsatisfied; 2, unsatisfied; 3, neutral; 4, satisfied; or 5, very satisfied). After transfer to the ward, all patients were administered 20 mg nefopam HCl in 100 ml of 0.9% saline IV for 4 hours.
Statistical analysis
The primary outcome was set as the intensity of pain at 6 hours after surgery. A sample size estimate indicated that 32 patients per group would provide a power of 80% (β = 0.20) at a level of 0.05 (α = 0.05) to detect a difference of 1 point on the VAS (0-10), with a standard deviation of 20, for each group in the preliminary test [
5]. After considering incomplete data collection and exclusion of patients (with a dropout rate of 10%), a total of 72 patients were included in the study. For statistical analysis, IBM SPSS 22.0 (IBM Corp., USA) was used. Results are presented as mean ± SD (parametric data), or as medians with ranges, and 25% and 75% percentiles (non-parametric data).
Data were analyzed using Student’s t-test (continuous variables with nearly normal distribution, such as patients’ ages, weights, heights, and opioid consumption), the Mann−Whitney U test (VAS scores and patients’ satisfaction with analgesia), and the chi-square test and Fisher’s exact test (categorical variables, such as American Society of Anesthesiologists physical status classification, number of rescue analgesic doses required, and adverse effects), as appropriate. Statistical significance was considered at a P value of < 0.05.
Hemodynamic variables, VAS, and PONV at each time point were compared using t-tests. Changes in hemodynamic variables, VAS, and PONV over time were compared between the groups using repeated-measures analysis of variance.
RESULTS
All surgeries were performed by the same surgeon. Seventy-two patients were randomly assigned to the two groups, and no patients were excluded from the study. There were no significant differences between patients in terms of demographic data, clinical characteristics, duration of surgery, and anesthesia. Time to recovery was significantly longer in group O than in group F (P = 0.021), but the difference was less than 10 minutes in terms of total anesthesia time; total anesthesia time was not clinically significantly different between the groups (
Table 1).
Table 1
Demographic Data and Anesthesia Characteristics
|
Variable |
Group F (n = 36) |
Group O (n = 36) |
P value |
|
Age (yr) |
39.4 ± 14.6 |
41.8 ± 14.3 |
0.903 |
|
Sex (M/F) |
23/13 |
21/15 |
0.629 |
|
Weight (kg) |
67.1 ± 11.8 |
63.7 ± 13.1 |
0.489 |
|
Height (cm) |
170.2 ± 8.6 |
167.8 ± 9.1 |
0.655 |
|
History of smoking |
5 (13.9) |
3 (8.3) |
0.710 |
|
History of PONV |
0 |
0 |
1.000 |
|
History of motion sickness |
0 |
0 |
1.000 |
|
ASA PS (I/II) |
26/10 |
24/12 |
0.609 |
|
Cormack-Lehane grade (1/2) |
33/3 |
32/4 |
0.693 |
|
Duration (min) |
|
|
|
|
Surgery |
51.9 ± 23.3 |
56.8 ± 29.2 |
0.330 |
|
Anesthesia |
68.2 ± 23.0 |
70.5 ± 28.7 |
0.316 |
|
Recovery |
6.9 ± 1.8 |
8.1 ± 2.8 |
0.021 |
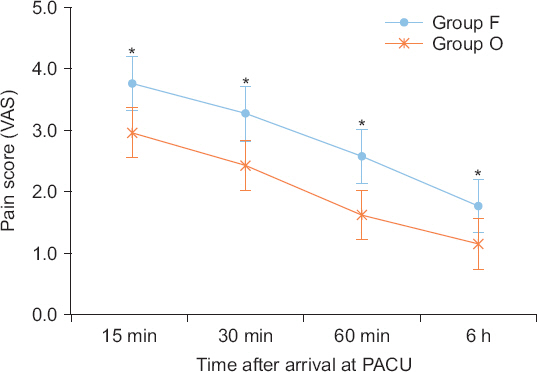
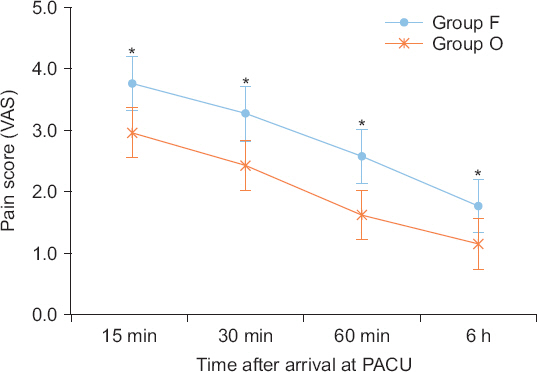
Comparison of the pain score using VAS at consecutive time points revealed that the pain intensity differed significantly between groups. The overall pain score was significantly lower in group O at all time points assessed in the PACU and at 6 hours after surgery (P < 0.001,
Fig. 1). While staying in the PACU, patients in group O were significantly less likely to require rescue analgesics (P = 0.032).
Fig. 1
Comparison of postoperative pain. Data are expressed as mean ± SD. Group F: fentanyl group, Group O: oxycodone group. VAS: visual analogue scale, PACU: post-anesthetic care unit. *P < 0.05 compared with Group O; VAS scores at each time point were compared using t-test.
The time to the requirement of the first rescue analgesic in group O was longer than that in group F, but this was not statistically significant. Postoperative complications in the PACU included PONV, headache, dizziness, sore throat, and respiratory depression. Neither group showed any serious complications or respiratory depression. In both groups, the incidence of postoperative complications was not significantly different, except for PONV (
Table 2). There was a significantly lower incidence of postoperative nausea in group O at 30 minutes and at 60 minutes after arrival in the PACU (
Table 3). Anti-emetic injections were administered to four patients in group F who had moderate PONV 30 minutes after arrival in the PACU and to one patient in group O who had moderate PONV 15 minutes after arrival in the PACU. The incidence of PONV was increased when the IV bolus of fentanyl as rescue analgesic was injected at 30 minutes after arrival in the PACU.
Table 2
Recovery Profile and Patient Satisfaction Score
|
Variable |
Group F (n = 36) |
Group O (n = 36) |
P value |
|
Rescue analgesic use |
10 (27.8) |
3 (8.3) |
0.032 |
|
Time to first rescue analgesic use (min) |
26 ± 13.5 |
30 ± 21.7 |
0.937 |
|
Complications |
|
|
|
|
Rescue anti-emetic use |
4 (11.1) |
1 (2.8) |
0.167 |
|
Respiratory depression |
0 |
0 |
1.000 |
|
Headache |
0 |
1 (2.8) |
0.317 |
|
Dizziness |
4 (11.1) |
4 (11.1) |
0.967 |
|
Sore throat |
7 (19.4) |
4 (11.1) |
0.329 |
|
Patient satisfaction score at discharge* (1/2/3/4/5) |
0/2/13/20/1 |
0/0/2/16/18 |
< 0.001 |
Patient satisfaction scores at discharge were also significantly higher in group O than in group F (P < 0.001,
Table 2). The changes in hemodynamic variables and sedation scale in the PACU were comparable between the two groups at all time points (
Fig. 2,
Table 4).
Table 3
Incidence of Postoperative Nausea
|
Observation time |
Severity of nausea |
Group F (n = 36) |
Group O (n = 36) |
P value |
|
15 min at PACU |
Mild |
2 (5.6) |
2 (5.6) |
0.472 |
|
Moderate |
0 (0) |
1 (2.8) |
|
|
Severe |
0 (0) |
0 (0) |
|
|
30 min at PACU |
Mild |
9 (25) |
4 (11.1) |
0.007 |
|
Moderate |
4 (11.1) |
0 (0) |
|
|
Severe |
0 (0) |
0 (0) |
|
|
60 min at PACU |
Mild |
12 (33.3) |
1 (2.8) |
0.007 |
|
Moderate |
1 (2.8) |
1 (2.8) |
|
|
Severe |
0 (0) |
0 (0) |
|
|
6 h after surgery |
Mild |
1 (2.8) |
1 (2.8) |
1.000 |
|
Moderate |
0 (0) |
0 (0) |
|
|
Severe |
0 (0) |
0 (0) |
|
Table 4
Changes in Sedation Scale
|
Observation time |
Sedation scale grade* |
Group F (n = 36) |
Group O (n = 36) |
P value |
|
0 min in PACU |
S |
0 (0) |
0 (0) |
0.642 |
|
1 |
0 (0) |
0 (0) |
|
|
2 |
20 (55.6) |
18 (50) |
|
|
3 |
16 (44.4) |
18 (50) |
|
|
4 |
0 (0) |
0 (0) |
|
|
15 min in PACU |
S |
0 (0) |
0 (0) |
0.416 |
|
1 |
3 (8.3) |
0 (0) |
|
|
2 |
17 (47.2) |
19 (52.8) |
|
|
3 |
16 (44.4) |
17 (47.2) |
|
|
4 |
0 (0) |
0 (0) |
|
|
30 min in PACU |
S |
0 (0) |
0 (0) |
1.000 |
|
1 |
27 (75) |
27 (75) |
|
|
2 |
9 (25) |
9 (25) |
|
|
3 |
0 (0) |
0 (0) |
|
|
4 |
0 (0) |
0 (0) |
|
|
60 min in PACU |
S |
0 (0) |
0 (0) |
1.000 |
|
1 |
34 (94.4) |
34 (94.4) |
|
|
2 |
2 (5.6) |
2 (5.6) |
|
|
3 |
0 (0) |
0 (0) |
|
|
4 |
0 (0) |
0 (0) |
|
Fig. 2
Changes in hemodynamic variables. Data are expressed as mean − SD in group F and mean + SD in group O. Group F: fentanyl group, Group O: oxycodone group. Initial: arrival in the operation room, 0, 30, 60 min: minutes after arrival in the post-anesthetic care unit.

DISCUSSION
Oxycodone has pharmacological features similar to those of strong opioids (e.g., morphine, hydromorphone, and fentanyl), but seems to have a stronger effect in actual use [
3,
4,
6,
7]. The onset of action of IV oxycodone is similar to that of fentanyl (about 2-3 minutes after administration), and is more rapid than that of morphine. The analgesic duration of a single bolus of oxycodone is about an hour longer than that of fentanyl [
3]. According to studies that have compared the effects of IV oxycodone and fentanyl, the minimum effective concentration and minimum effective analgesic concentrations of oxycodone may vary, depending on the type of surgery [
4,
6,
8].
When comparing the efficacy of the drugs without changing the route of administration, measurements must be made at equi-analgesic doses [
1]. Oxycodone has shown a better analgesic effect when a potency ratio of oxycodone and fentanyl was assumed to be 100:1 after laparoscopic cholecystectomy, but the side effects also increased [
3]. In a recent comparison of equi-analgesic dose between oxycodone and fentanyl, the potency ratio to fentanyl was described as 60:1 after gynecological surgery [
4]. In our preliminary study, based on previous studies, the analgesic efficacy of oxycodone was excellent, but the incidence of sedation and PONV was high, at a potency ratio of 60:1 after dental surgery. Therefore, we used a potency ratio of 50:1 for this study of acute postoperative pain after surgical extraction of mandibular teeth.
Mandibular molar extraction has been used as an index to assess the effects of various anesthetics and sedatives on pain associated with surgical procedures, and its pathophysiology is similar to those of other types of acute moderate or severe pain. Acute pain after surgical extraction has homogenous pain stimulus and can be debilitating. Participants in dental surgery are relatively young and healthy subjects, which reduce confounding factors that may affect analgesic response. Moreover, dental surgery has no multiple surgical complications. Surgical extraction allows control over the surgical technique and the anesthesia method simultaneously and is therefore advantageous for titrating drug concentrations. The efficacy of an agent in the dental pain model is theoretically predictive of its effects in later stage models [
9-
11].
We focused on reducing the use of additional opioid analgesics in the PACU and maintaining longer analgesic effect to induce rapid recovery without opioid-related complications. Oxycodone has an advantage over fentanyl in terms of a longer analgesic duration based on a potency ratio of 50:1 in dental surgery. After a single IV bolus administration, fentanyl may not have sufficient analgesic action over an extended period. The time to the requirement of the first rescue analgesic was longer with the use of oxycodone, but it did not differ significantly from that with the use of fentanyl. Nevertheless, the actual number of patients requiring a rescue dose was significantly higher in the fentanyl group, indicating that oxycodone had a longer-lasting analgesic effect in the PACU than fentanyl. Our analysis demonstrates that about 1 point of VAS is considered clinically significant, but the minimal important difference as the smallest change correlates with the result of the questionnaire related to acute pain management at discharge. The patient satisfaction score for oxycodone was significantly higher than that for fentanyl.
Repetitive administration of opioid analgesic is a predictive factor of PONV. Therefore, anesthesia strategies that reduce administration of opioids are an effective means of reducing the incidence of PONV. We used a single IV bolus of opioid analgesic before the end of surgery; the frequency of additional injections was significantly lower in group O than in group F, and the reduced use of opioids may have resulted in the low incidence of PONV.
The analgesic efficacy of oxycodone has not been clearly established; some studies have demonstrated that oxycodone has markedly increased analgesic efficacy over that of other opioids [
3,
4,
6,
8,
12]. Although oxycodone caused more PONV than fentanyl in other studies, we verified that oxycodone was not disadvantageous in terms of the development of PONV. Moreover, a single bolus of IV oxycodone was more effective for acute post-operative pain relief by maintaining longer analgesic activity in the PACU. Therefore, various experiments need to be conducted to identify the appropriate dose of oxycodone for treatment of different types of pain.
Our study has some limitations. First, we did not compare the analgesic effects of oxycodone and fentanyl for the subacute period or in a continuous fashion after discharge. The main focus of the study was the assessment of acute pain relief in the PACU, and subsequent control of subacute analgesic effects was not possible. Because of the nature of this type of surgery, most patients were discharged after 24 hours, and the possibility of transitioning to chronic pain could not be investigated. Second, only healthy patients were included in our study. Metabolic clearance of oxycodone is affected by lean body mass and age, as critical covariates; with increasing age and decreasing lean body mass, steady-state concentrations of the drug are maintained at higher levels [
7]. Further studies should be conducted in patients with diverse demographics and various clinical features [
13].
In conclusion, in a concentration of 0.05 mg/kg IV oxycodone and 1 μg/kg IV fentanyl, oxycodone had more favorable analgesic efficacy for acute postoperative pain, without additional rescue analgesics, after dental surgery. Thus, oxycodone is considered a valuable alternative opioid analgesic to improve the quality of patient analgesia.