Vertebroplasty of compression fracture with prevertebral hematoma during treatment of postherpetic neuralgia -A case report-
Article information
Abstract
Postherpetic neuralgia (PHN) and vertebral compression fracture (VCF) are common causes of chronic pain in the elderly population. Careful history taking and imaging studies are needed for diagnosis when both diseases coexist. Vertebroplasty is a clinically efficient surgical treatment of VCF, while nerve block and/or medications are the mainstay of PHN pain control. The most serious complications of vertebroplasty are pulmonary embolism or neurologic deficit due to cement leakage. An 80-year-old female patient was diagnosed with PHN of the right L1 dermatome; however, her pain expanded to the midback and subcostal area. Thoracic magnetic resonance imaging and abdominal computed tomography revealed recent L2 compression fracture with prevertebral hematoma caused by cortical bone defect of the L2 body. Even though the risk of cement leakage was high, L2 vertebral body augmentation was performed using a bone filler device and high-viscosity cement; this treatment was successful, without cement leakage or any other complications.
INTRODUCTION
The most common cause of vertebral compression fracture (VCF) is osteoporosis in elderly women. Herpes zoster is also common among the elderly population as immunity to the varicella zoster virus wanes. There are differences in the pain characteristics of VCF and PHN. Pain from postherpetic neuralgia (PHN) is usually unilateral and single dermatomal rash with pain; patients sometimes complain of superficial pain as well as deep pain. Pain from VCP is usually bilateral, deep, and occurs in segmental area of the back. Movement aggravates VCF pain, while it rarely influences PHN pain.
The risk factors for cement leakage during vertebroplasty include a large volume of injected cement, cortical bone disruption, intravertebral cleft, high fracture severity, and low polymethylmethacrylate bone cement viscosity [1,2]. The patient in the present case reported PHN in the right L1 dermatome, but complained not only of right L1 dermatomal pain, but also of midback, subcostal, and bilateral abdominal pain caused by L2 VCF with abdominal hematoma and cortical bone defect. Although the risk of cement leakage following vertebroplasty was high because of L2 anterior cortical defect, L2 vertebroplasty was successfully performed using a bone filler device and high-viscosity cement without cement leakage.
CASE REPORT
An 80-year-old female patient was diagnosed with herpes zoster on the right first lumbar nerve two months prior in another clinic and had been taking medication for persistent pain since then. When herpes zoster first occurred, she experienced shooting and pricking pain in the right flank and inguinal area with a vesicular rash on the right L1 dermatome. After one month, the pain spread to her midback and both subcostal and abdominal areas, and was aggravated by truncal movement, while right L1 dermatomal shooting pain continued. On physical examination, the patient reported mild hypesthesia on the L1 dermatome without allodynia where she was already diagnosed with PHN, and moderate tenderness on the lower thoracic and lumbar spine. The clinical impression was of VCF and PHN. Patients with vertebral compression fractures do not typically complain of persistent shooting pain while resting; however, this patient reported persistent shooting subcostal and abdominal pain and superficial like PHN. Since her pain had changed and expanded over the prior 2 months since diagnosis of PHN, radiological imaging study was performed to rule out VCF (Figs. 1A and 1B). Thoracic magnetic resonance imaging revealed recent compression fracture of the L2 vertebral body and hematoma in the prevertebral space between T12 and L2 (Fig. 2). Abdominal computed tomography (CT) ruled out other possible causes of hematoma. Abdominal CT confirmed cortical breakage of the L2 at the right anteroinferior corner of the vertebral cortex and prevertebral hematoma between T12 and L2 (Fig. 3). T-score is −2.9 measured by bone mineral density test. Thus, we concluded that the hematoma was the result of cortical bone disruption of the L2 vertebral body. The risk of cement leakage was high due to anterior cortical bone disruption of the L2 vertebral body; however, we decided to perform L2 vertebral augmentation because the patient was suffering intractable pain despite conservative treatment.
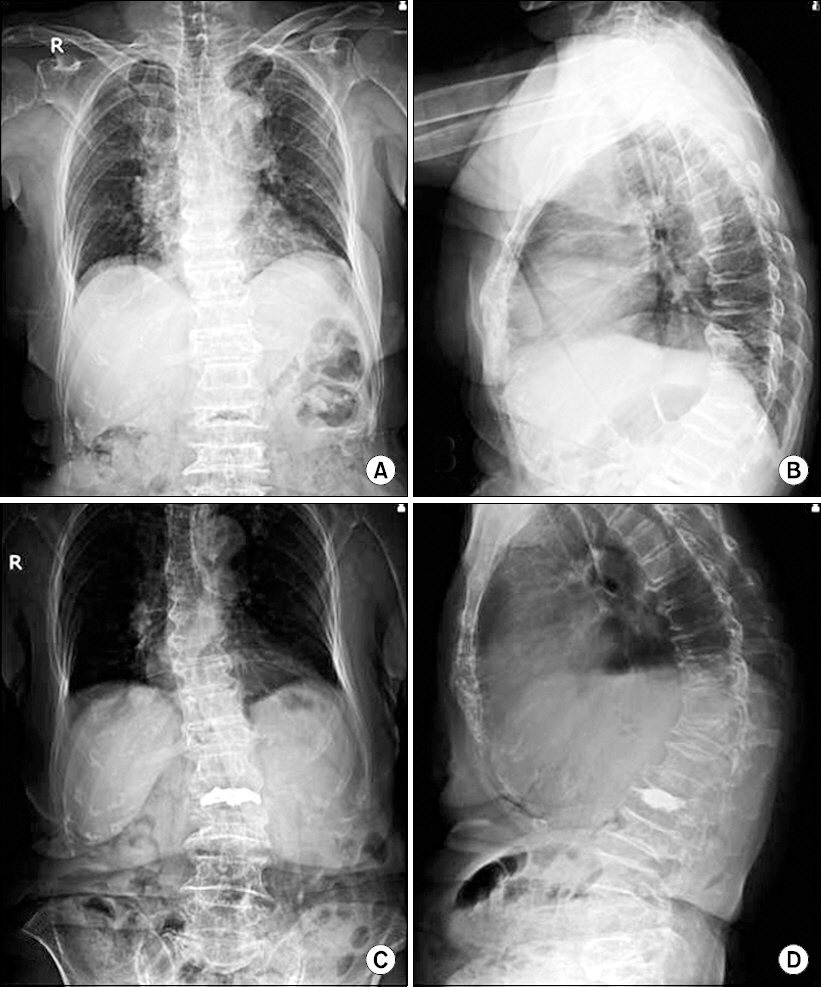
Anteroposterior and lateral radiographs before (A, B) and after (C, D) vertebroplasty of the L2 vertebral body. (A and B) show T12 and L2 compression fracture with intravertebral vacuum of L2 body. (C and D) show bone cement fills the fractured vertebra without leakage.
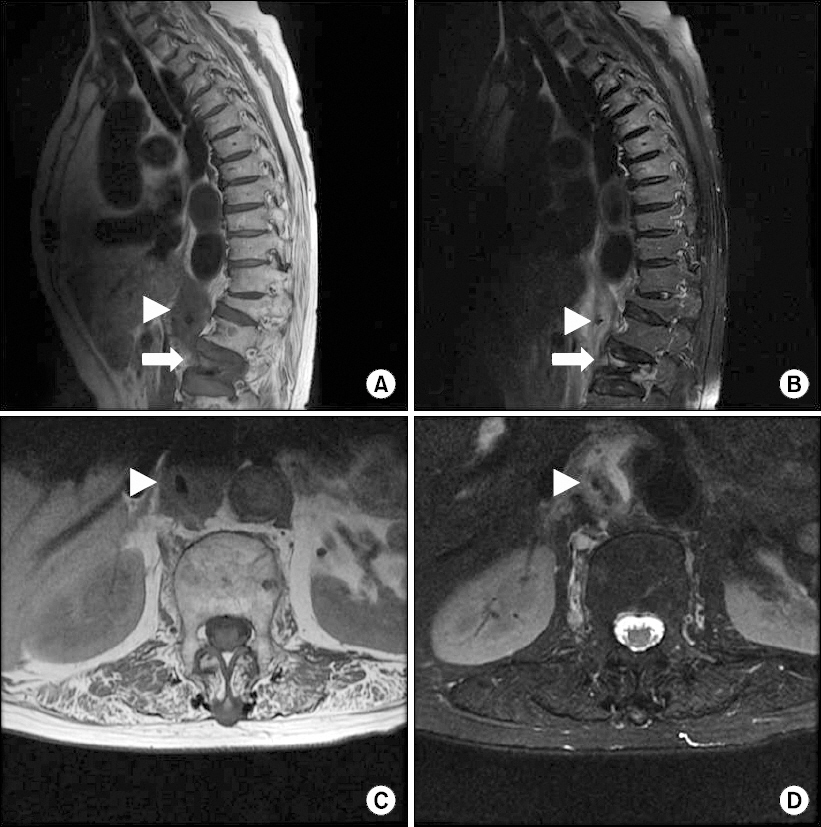
Thoracic spine-MRI shows recent L2 compression fracture (arrow) with intravertebral vacuum and paravertebral hematoma (arrow head) with an 8.3 × 3 × 2.6-cm heterogeneous signal intensity in the prevertebral area adjacent to the abdominal aorta between T12 and L2. (A) T1-weighted sagittal image, (B) T2-weighted sagittal image, (C) T1-weighted axial image at the L1 level, (D) T2-weighted axial image at the L1 level.
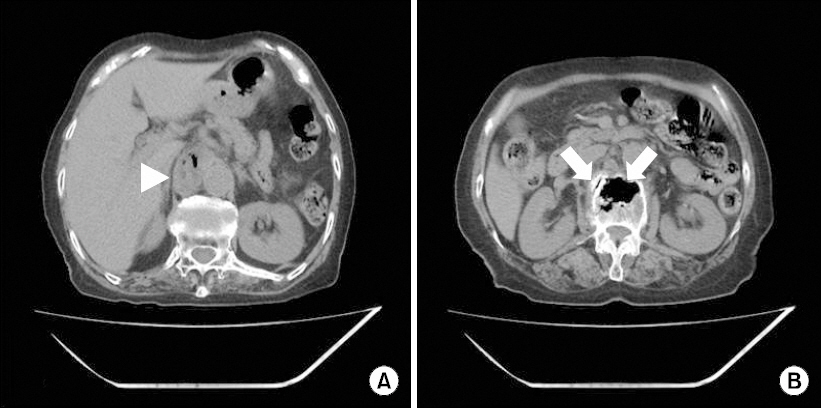
(A) Abdominal CT reveals a prevertebral nonenhancing soft tissue mass with heterogeneous density and intralesional multiple gas shadow between the inferior vena cava and the proximal abdominal aorta (arrow head) at the upper L1 level. (B) Intravertebral vacuum of L2 with cortical breakage (arrow) at the anteroinferior corner.
The patient was placed in the prone position. After aseptic preparation, a bone biopsy needle was inserted, targeting the slightly upper and lateral side of the left pedicle of the L2 vertebral body, under the AP view of the fluoroscope. The needle was advanced into the anterior side of the posterior cortex of L2 under the AP and lateral view of the fluoroscope alternatively. A guide wire was inserted through the bone biopsy needle hole and a working cannula was advanced over the guide wire into the anterior side of the posterior cortical bone. After removing the stylet of the working cannula, a cortical blunt dissector was advanced to the anterior one fourth of the L2 vertebral body under lateral view fluoroscopy. The same procedure was done on the right side. Then, bone cement was injected through a bone filler device. Due to the intravertebral vacuum and anterior cortical breakage present in the L2 vertebral body, we waited for the viscosity of the mixed cement to become high enough for it to maintain its cylindrical shape as it came out of the bone filler device (HDS SYSTEM, Han-Song Biobank, Korea) (Fig. 4). Five milliliters of cement were slowly injected into the vertebral body over 3 minutes (Figs. 1C and 1D). On the day after the procedure, the patient reported nearly complete resolution of midback and subcostal pain previously aggravated upon truncal movement and abdominal pain was decreased by 70%. The patient was discharged without complications.
DISCUSSION
The risk of PHN and VCF increases with age. Among elderly patients receiving treatment for herpes zoster, compression fracture of the spine is not uncommon. Choi et al. [3] reported a case wherein compression fracture of the spine was diagnosed when applying C-arm fluoroscopy transforaminal block to treat herpes zoster; vertebroplasty was performed to address compression fracture. In the present case, one month after shooting pain in the right flank and inguinal area led to diagnosis of herpes zoster, midback pain aggravated by truncal movement and bilateral subcostal and abdominal pain appeared. Based on the pain characteristics and patient age, we suspected VCF at the lower thoracic level. L2 compression fracture and concomitant prevertebral hematoma (8.3 × 3 × 2.6 cm) were found, which could have provoked subcostal and abdominal pain similar to the previously described herpes zoster-related pain.
Vertebroplasty can be very helpful in cases where conservative treatment is insufficient to control VCF pain. It is an effective treatment modality not only for pain control, but also for vertebral height restoration, compression ratio reduction, and segmental Cobb’s angle reduction [4,5]. Despite these advantages, if VCF is severe, technical difficulty and increased risk of cement leakage can lead to negative outcomes of vertebroplasty. Contraindications to vertebroplasty are coagulopathy, rupture of the posterior wall of the vertebral body, cement allergy, pregnancy, and grade III collapsed vertebra.
Cement leakage is a common complication of vertebroplasty, but it is rarely symptomatic. According to a study by Weill et al. [6], 20 (38.4%) of 52 patients had cement leakage into the epidural fat, perivertebral soft tissue or epidural vein, but only 5 patients exhibited symptoms of cement leakage. Cement leakage to the adjacent disc is asymptomatic, but can lead to long-term mechanical consequences of adjacent vertebral body [7]. Serious complications of cement leakage such as spinal cord compression, pulmonary embolism, and radicular pain are very rare; however, these complications can be life threatening or can lead to permanent neurologic deficits [8]. High fracture severity grade, low cement viscosity and high injection pressure are strong independent risk factors for cement leakage [1,9]. The use of medium- instead of low-viscosity cement reduces the risk of leakage by more than 25% [1]. In comparison to kyphoplasty, vertebroplasty is associated with a higher risk of cement leakage because of the higher injection pressure, lower cement viscosity and smaller needle diameter. If a bone filler device with larger diameter is used instead of 1 ml tuberculin syringe for injecting cement, higher viscosity cement could be injected with lower pressure. However, there has been no clinical study that make a comparison between traditional method and vertebroplasty with bone filler device. Yang et al. [10] concluded that vertebroplasty with a bone filler device achieves similar compression reduction and even greater sponge-type bone cement distribution with similar risk of bone cement leakage in comparison with balloon kyphoplasty. Therefore, a large-diameter bone filler can reduce the risk of cement leakage, since it allows the use of bone cement with high viscosity and low pressure injection.
In this case, there was a cortical defect with prevertebral hematoma and the potential risk of bone cement leakage was high. However, we reduced the risk of cement leakage during vertebroplasty by using a bone filler device to inject high- viscosity bone cement. Injecting the appropriate volume of cement is important to restore the strength and stiffness of the compressed vertebral body and to prevent cement leakage. Excessive cement volume can increase the risk of cement leakage and lead to excessive stiffness and adverse outcomes. Just 2 ml of cement can restore the strength of the spine and 4–8 ml of cement can restore the stiffness [11]. In this case, 5 ml of bone cement was injected. The risk is increased if there are cortical defects and abnormally high signal intensity in the adjacent disc on T2WI [12]. In contrast, Lee et al. [13] suggested that low signal intensity linear lesion of the intervertebral disc is a more accurate and useful predictor of leakage.
In conclusion, we recommend that thorough physical examination and history taking be performed to rule out any other causes of previously diagnosed PHN in elderly patients, especially when pain characteristics change or progress. We carried out vertebroplasty using a large-diameter bone filler in a VCF patient with prevertebral hematoma due to cortical bone defect. We achieved a good outcome, reducing pain without complications. Therefore, this method of vertebroplasty may be useful in patients at high risk of cement leakage.
