INTRODUCTION
Spinal problems are a common pathology in women of child-bearing age. The prevalence of low back pain (LBP) during pregnancy is known to be more than 50% in many studies. Symptomatic lumbar disc herniation is one of the most common spinal problems during pregnancy, which occurs at a frequency of approximately 1 in 10,000 pregnancies. Because delayed diagnosis or treatment can cause permanent neurologic deficits, pregnant women who complain of LBP or radiating pain should be examined carefully and in a timely manner [1]. In this report, we present the case of a pregnant woman complaining of LBP with radicular pain and successful management of her pain using ultrasound (US)-guided pararadicular block.
CASE REPORT
A 30-year-old woman had been pregnant for 18 + 5 weeks when she visited our pain clinic. The patient complained of LBP with radiating pain to the posterolateral side of her right leg. Two years previously, she had attended a neurosurgery department for aggravation of LBP without radiation. At that time, magnetic resonance imaging showed a diffuse bulging disc at L4-5 with an annular fissure, anterolisthesis at L5-S1, and mild neural foraminal stenosis on the left side. She had recovered from her previous symptoms after receiving a lumbar epidural block.
Physical examination was performed, revealing a negative Patrick sign and a positive straight leg raising sign on the right side. The pain was aggravated by flexing her back when she turned to the right side while lying down. Her pain on a numeric rating scale (NRS) was 5-6 out of 10. No further imaging was done due to her pregnancy. Instead, US-guided pararadicular block (with 5 ml of 0.2% lidocaine) using a paramedian sagittal oblique approach was performed.
The patient was placed in a left lateral decubitus position. After draping the skin from the mid lumbar area to the iliac crest in a sterile fashion, the transducer was positioned over the skin to identify the L4-5 intertransverse ligament. First, the fifth lumbar spinous process and the first sacral spinous process were identified in the median plane by longitudinal placement of the transducer (Fig. 1A). The spinal level was determined by counting cephalad from a break between the fifth lumbar spinous process and the uninterrupted hyperechoic sacrum. Then, the transducer was moved laterally, showing the lamina, the zygapophyseal joint, and the transverse process in that order. The transducer was moved back toward the midline to visualize the zygapophyseal joint (Fig. 1B). In this final scanning plane, we could find the image of the intertransverse ligament. In prior studies, this plane was referred to as the “pararadicular aditus plane” [2,3]. By tilting the transducer 20-25° (using the paramedian sagittal oblique technique), the needle was advanced in-plane (Fig. 1C). In this injection plane, the intertransverse ligament appeared as a hyperechoic band between the two adjacent transverse processes. The pararadicular compartment is beneath the intertransverse ligament, which lies next to the lumbar nerve (Fig. 2). Because lumbar nerves are poorly visible on sonography, the intertransverse ligament was chosen as the needle path. The needle was advanced until the intertransverse ligament was punctured [2]. Two milliliters of 0.2% lidocaine was injected as a trial. After 3 min, the remaining 3 ml was injected after confirming no indications of vital sign fluctuation, seizure, nausea, or eyesight blurring, which might occur as consequences of intravascular injection or local intoxication.
Fig. 1
(A) Placement of transducer using the paramedian sagittal oblique technique. (B) Ultrasound (US) image showing pararadicular injection at the level L4-5. (C) US image showing pararadicular injection at the level L4-5 with annotation.
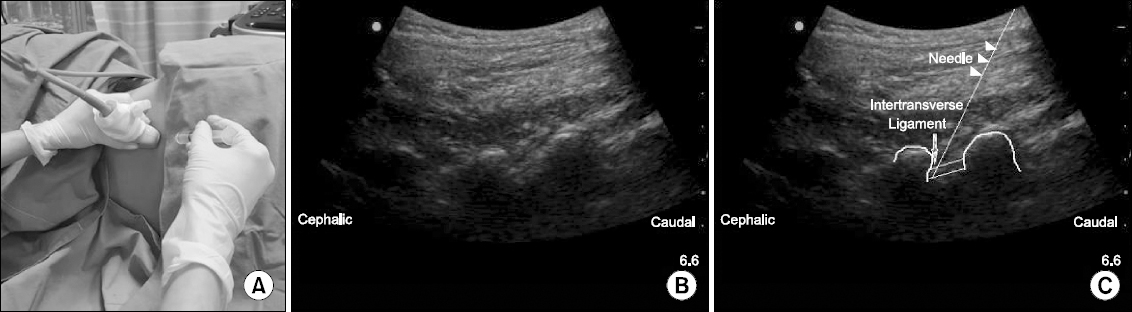
Fig. 2
Lumbar spine model showing paramedian sagittal oblique approach targeting the intertransverse ligament indicated as a black plastic structure between two adjacent transverse processes.

After the block, the patient’s lumbar and leg pain decreased to 0/10 on the NRS. Her vital signs were stable throughout the procedure. When the patient returned to our clinic 2 months later, her NRS score was still 0/10. At postconceptional week 38 + 5, labor was induced and the patient gave birth without complication.
DISCUSSION
Lumbar pain is typically treated via transforaminal epidural injections, which have been preferentially performed under fluoroscopic or computer tomography (CT) guidance [3]. However, both guidance modalities deliver significant doses of radiation that may interfere with the development of a fetus [4]. The formation of the fetal central nervous system occurs primarily during the last 6 months of pregnancy. Because this period is long and involves increasing physical stress on the mother, injuries are more probable during this phase. Exposure to radiation above a certain threshold dose may lead to substantial mental retardation as well as a decrease in intelligence quotient (IQ) among affected children [4]. It may also result in malignant disorders [4].
Previous studies have examined US-guided nerve root block and transforaminal injections and compared them to other, more conventional techniques. Loizides et al. [3] evaluated the accuracy, overall pain relief, and time-savings of US-guided lumbar pararadicular injections compared to a CT-guided approach. The authors observed no significant difference between the US- and CT-guided groups regarding patient perception of pain relief, but the mean time to fine needle placement in the US group was approximately half that of the CT group. In 90% (18/20) of the US-guided cases, the correct needle placement was confirmed by the subsequent CT image [3].
There are several methods used in US-guided lumbar root blocks. Kim et al. [2] used fluoroscopy to investigate the dispersal of the anesthetic agent after US-guided injection via either a paramedian sagittal oblique approach or paramedian sagittal approach. The pattern of contrast dispersal was evaluated as being extraforaminal vs. intraforaminal, ventral vs. dorsal epidural, and extraepineural vs. intraepineural. Among the successful pararadicular injections, an intraforaminal contrast pattern was found in 87.5% (35 cases) of those treated via the paramedian sagittal oblique approach, compared to only 39.5% (17 cases) of those treated via the paramedian sagittal approach. In addition, pain perception evaluated using a visual analog scale (VAS) was much lower in the paramedian sagittal oblique group [2]. These results suggest that the paramedian sagittal oblique approach resulted in improved intraforaminal flow, leading to better pain relief.
The intraforaminal space is connected to the ventral epidural space and is the most common site of pathology in disc herniation. Ventral epidural flow was achieved in most cases of intraforaminal flow. In the paramedian sagittal oblique group, the needle was placed more medially compared with the paramedian sagittal group, thus enhancing the spread of contrast material into the intraforaminal and ventral space [2,5]. The difference in postprocedural VAS score may be attributed to greater intraforaminal distribution. In this case of a pregnant patient, we also chose the paramedian sagittal oblique approach due to its high probability of successful intraforaminal distribution. The method was expected to cause less nerve irritation compared to the previous approach designed by Gofeld [6,7] because the injection targeted a new landmark. By using the hyperechoic intertransverse ligament as a landmark instead of the poorly visible lumbar roots, the injection was much easier and safer. US-guided pararadicular block using a paramedian sagittal oblique approach might be a reasonable alternative to fluoroscopy-guided epidural blocks in certain populations, including pregnant women.
In addition to methods of approach, the concentration of local anesthetic used in the lumbar block is another concern during pregnancy. Half of epidural lidocaine is absorbed into systemic circulation within 100 min of injection, and more than 5 μg/ml plasma lidocaine may lead to complications such as lightheadedness or numbness [8]. The effective analgesic dose of lidocaine is 1-5 μg/ml [8]. Previous studies have compared the effects of administering equal doses of solutions at different concentrations [9]. However, there is no consensus regarding the minimum effective dose of lidocaine, so we empirically chose the lowest effective dose for safety reasons.
We also used a dilute lidocaine solution to prevent any potential harm to the fetus. The US Federal Drug Administration (FDA) has assigned lidocaine to pregnancy category B, meaning that neither animal nor human studies show evidence of fetal harm. However, use is not recommended unless clearly needed. Lidocaine crosses the human placenta rapidly and may be related to decreased Apgar scores, apnea, fixed and dilated pupils, and seizures in neonates [10]. Plasma concentrations of alpha-1-acid glycoprotein are also decreased in pregnant women and newborns, subsequently increasing the free fraction of local anesthetic in plasma. Moreover, dilated epidural veins during pregnancy may contribute to the decreased volume of epidural space, thus resulting in more extensive spread of local anesthetic. Based on the current research, the dose of lidocaine used during pregnancy should be reduced by at least 30%, despite its intermediate duration of action [11,12]
Here, we present the case of a pregnant patient with worsening LBP who was successfully treated using US-guided lumbar root block. Pararadicular block using a paramedian sagittal oblique approach with a reduced amount of anesthetic may be a good alternative to fluoroscopically guided block for lumbar pain during pregnancy.








