Concurrent meralgia paresthetica and radiculopathy of the left leg -A case report-
Article information
Abstract
Meralgia paresthetica (MP) is a painful mononeuropathy of the lateral femoral cutaneouse nerve (LFCN) characterized by localized symptoms of numbness, tingling, pain and paresthesia along the anterolateral thigh area. L4 and L5 radiculopathy is set of symptoms that include sharp, burning or shooting pain, which is usually localized to anterolateral leg area and along the dermatomal distribution. When symptoms of MP and lumbar disc disease occur together it is not easy to diagnose MP. We report a case of synchronous post-traumatic MP and radiculopathy due to intervertebral disc herniation at L3–4 and 4–5. A 59-year-old male patient was admitted to the emergency room with symptoms of low back pain with left severe L4, L5 radiculopathy. This patient also complained of numbness and paresthesia in the left anterolateral thigh. After detailed history taking and lateral femoral cutaneouse nerve block, he was diagnosed with MP.
INTRODUCTION
Meralgia paresthetica (MP) is a sensory mononeuropathy of the lateral femoral cutaneouse nerve (LFCN), which is commonly due to focal entrapment of this nerve as it passes through the inguinal ligament [1-3]. However, corresponding presentations in the same area of both MP and L4, L5 radiculopathy is rarely reported, especially if patient is non-obese. Therefore, proper examination and correct diagnosis are not easy. The present case is a patient who was considered to have an ordinary lumbar disc herniation but was also found to have MP by detailed examination and history taking. We herein report a rare case of concurrent MP in a patient with lumbar disc herniation.
CASE REPORT
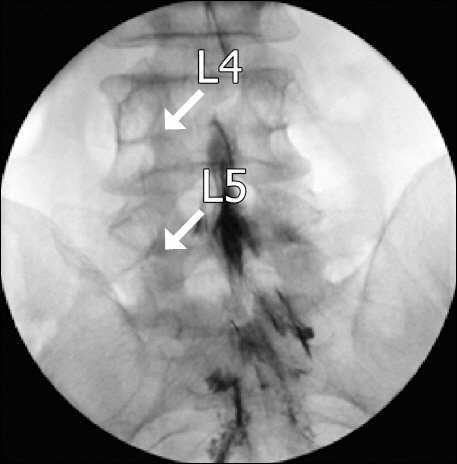
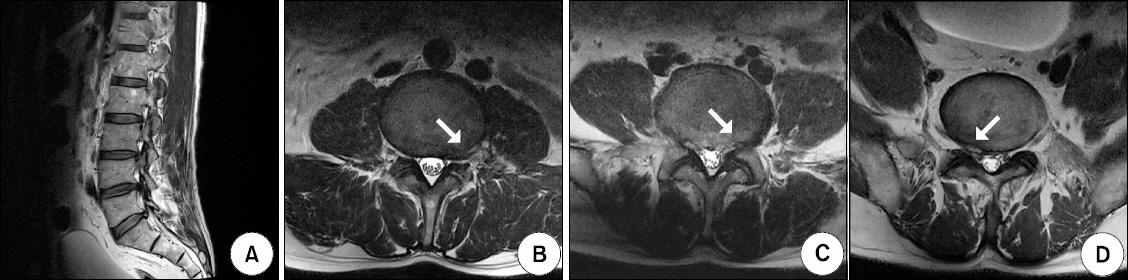
A 59-year-old male patient was admitted to the emergency room with symptoms of lower back pain, severe pain and a tingling sensation of the left anterolateral thigh, knee and anterior part of lower leg, numbness of the left foot dorsum and big toe, and paresthesia in the left anterolateral thigh; all that had been exacerbated after playing golf that morning. The patient reported baseline numbness that began after climbing a mountain 7 days before. At the time of admittance, the patient was bedridden and could not walk due to severe pain, rated 7/10 on the numeric rating scale (NRS). A neurological examination revealed no weakness or abnormality in his reflexes. His height was 174 cm and his weight was 70 kg, with body mass index of 23.13 kg/m2. His past medical and surgical history were unremarkable. Lumbar magnetic resonance imaging revealed L3-4-5-S1 stenosis, L3–4, L4–5 and L5–S1 disc degeneration, left foraminal disc protrusion at L3–4, left subarticular disc protrusion at L4–5 and right paracentral disc protrusion at L5–S1 (Fig. 1). The next morning, he was referred to our pain clinic. We planned to perform caudal epidural steroid injection (ESI). After informed consent for ESI was obtained, the patient was brought to the fluoroscopy room and placed prone on the table. However, the epidurogram showed a filling defect of the left L4, L5 nerve roots (Fig. 2). Thus, we performed fluoroscopically guided transforaminal ESIs at the level of the L4, L5 spinal nerve roots using 5 mg of dexamethasone, 0.3% lidocaine 5 ml and hyaluronidase 1,500 IU instead of caudal ESI (Fig. 3). Three days after the procedure, pain intensity of the lower back and left leg radiculopathy (severe pain and tingling sensation of left anterolateral thigh, knee and anterior part of lower leg, numbness of left foot dorsum and big toe) of the patient decreased from a NRS ranking of 7/10 to 3/10. The patient remained unable to walk because of a tingling sensation in the anterolateral thigh and continued paresthesia. Under the high suspicion of another disease, further evaluations were done. Through additional history taking, the patient recalled slightly bumping his left inguinal area on a tree during a climbing expedition. Physical examinations revealed tenderness over the lateral inguinal ligament, the motion of hip flexion and a pelvic compression test made the patient feel relaxed of symptoms after 45 seconds. Based on past history, symptoms and physical examinations, post-traumatic MP was suspected, so an ultrasound-guided LFCN block was planned for diagnostic and therapeutic purposes. The patient was placed in the supine position with the monitor applied. The target area was prepared and draped in a sterile fashion. Using a LOGIQ e ultrasound machine (GE Medical Systems, China), a linear 6–13 MHz transducer was placed on the anterior superior iliac spine (ASIS) and moved down medial and inferior. The LFCN was located in between the tensor fascia lata and the sartorius muscle was identified as a hypoechoic structure. After identification of the LFCN, A 23-gauge, 6-cm needle was advanced in-plane until it was positioned near the LFCN. A mixture of a total volume 6 ml of 1% lidocaine containing 2.5 mg dexamethasone was injected around the LFCN with ultrasound monitoring (Fig. 4). After the LFCN block, the patient stood up in 30 minutes. The pain intensity ultimately decreased to a NRS rating of 1/10. When he was discharged, he was able to walk without assistance. Also, his left anterolateral thigh pain measured on a NRS had decreased by 90% and the tingling sensation and paresthesia of the left leg had improved substantially. After 6 weeks follow-up, the improved condition of patient has continued without complications.
Sagittal T2-weighted magnetic resonance imaging (MRI) showing L3-4-5-S1 stenosis, L3–4, L4–5 and L5–S1 disc degeneration (A). Axial view of MRI shows left foraminal disc protrusion at L3–4 (B), left subarticular disc protrusion at L4–5 (C), and right paracentral disc protrusion at L5-S1 (D).
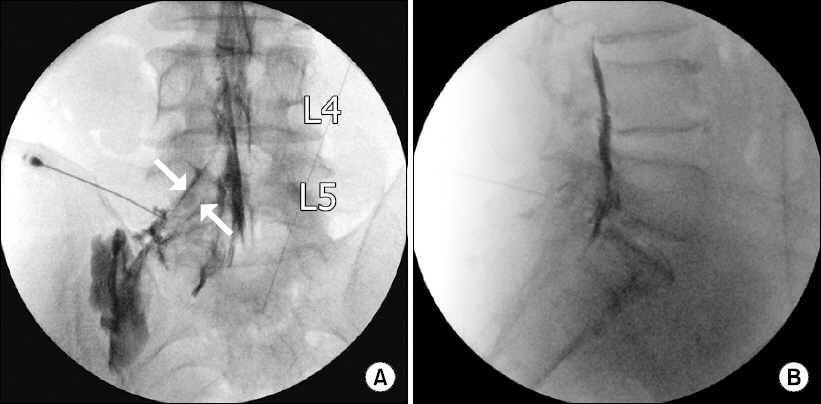
An anteroposterior live fluoroscopic image taken during a contrast injection for a left L5 transforaminal epidural steroid injection (A). Lumbar lateral view revealing a contrast medium in the anterior epidural space (B).
DISCUSSION
LFCN entrapment is not commonly accompanied with L4, L5 radiculopathy [4]. However, this case highlights the fact that these two symptoms can coexist. MP is a sensory mononeuropathy of the LFCN, which is purely sensory; common clinical symptoms are characterized by tingling, numbness, pain and paresthesia in anterolateral thigh area without motor symptoms or reflex deficits [2,5]. Usually, MP symptoms are typical and consistent, in which paresthesia is localized to LFCN and activities such as walking and descending the stair can aggravate the symptoms, because these activities require extension of the hip and stretching the nerve [6]. These symptoms result from entrapment or compression of the LFCN, which arises from the 2nd and 3rd spinal nerve of the lumbar plexus, and transits between the inguinal ligament and the ASIS [3]. It can develop primarily by increasing abdominal pressure caused by obesity, pregnancy, pelvic mass, tight clothes, metabolic disease and diabetes mellitus, or can be caused secondarily by surgical procedure or local trauma [7]. MP can be suspected based on medical history indicating that the symptoms are exacerbated by extension of the hip and relieved by flexion of the hip in specific postures, or by physical examination like the pelvic compression test [6,8,9]. A pelvic compression test is useful as a screening test for MP. The examiner presses the lateral side of the pelvis for 45 seconds and asks whether any symptoms have been relieved. If the symptoms are relieved, the result of the test is regarded as positive [6,9]. In addition, the screening test is useful in gauging tenderness on the lateral inguinal ligament where the nerve bypass is detectable during physical examination [1]. MP is purely sensory and does not follow dermatomal distributions, in contrast to intervertebral disc herniation, in which there may be reflex or motor deficits. In a patient with MP, there should be no positive response to the straight‐leg‐raising test or sciatic notch tenderness [10].
However, it was difficult to suspect MP directly in this patient because his medical and surgical history was clear, the lack of obesity and his description of a tingling sensation, numbness, paresthesia of the left leg and low back pain with left L4, L5 radiculopathy at the same time. Lumbosacral radiculopathy is characterized by low back pain with radiating pain, which may be accompanied by sensory loss, tingling sensation and pain [11,12]. Many examples and studies have been reported on the causes, diagnosis and the treatment of MP, but cases of having these two symptoms together have been rarely reported. When the patients are appealing the distinct pain followed with L4, L5 dermatome distributions, we had never thought about possibility of MP. However, presently, when the leading symptom was relieved from the knee to the great toe after L4, L5 transforaminal ESIs, he still had paresthesia in the anterolateral thigh. In a careful examination and history-taking, the patient disclosed having bumped slightly into a tree with the left inguinal area when mountain climbing 7 days prior to coming to the emergency room. And the patient showed a positive finding in the physical examination associated with it. When patients complain of a tingling sensation and paresthesia of the anterolateral thigh, metastasis at the iliac bone [13] and lumbar disc herniation [4] should be ruled out. Lesions involving the lateral hip area such as the trochantric bursitis, and gluteus medius muscle dysfunction and iliotibial band syndrome should be differentially diagnosed [14].
Most cases of MP follows a benign course and 85% of patients recover with conservative treatment that includes avoidance of compressing factors, application of oral medication (nonsteroidal anti-inflammatory drugs, tricyclic antidepressants, anticonvulsant, antiarrhythmic) for neuropathic pain [15]. However, active treatment, sono-guided LFCN block or surgical intervention, such as neurolysis, transposition and transection of LFCN, is sometimes needed [10].
In this case, another diagnosis may be forthcoming when immediate improvement of symptoms is shown through sono-guided diagnostic LFCN block. The prognosis and the progress of MP is worse in patients with disc herniation than in patients without disc herniation. In the present case, the patient was unable to walk before both transforaminal nerve block and LFCN block were done. Several types of disease can occur in the same patient. Thus, it is important to identify the origin and type of pain to find the appropriate treatment. Final diagnosis must be based on medical and past history, clinical examination, imaging of lesion and pain. Complaint of symptoms of Left L4, L5 radiculopathy and MP should prompt diagnosis and treatment based in part on careful history taking. Stereotypical thinking can overlook something important. Therefore, physicians should keep in mind that several diseases can be present and need to examine patients more carefully, with history taking providing valuable clues.