INTRODUCTION
A patient presenting with a large anterior mediastinal mass is a substantial challenge for anesthesiologists, especially when the patient experiences dyspnea in the supine position. Total occlusion of the airway and cardiovascular collapse are well- recognized complications in such patients during general anesthesia [
1-
3], yet diagnostic procedures, including computed tomography (CT)-guided percutaneous needle biopsy or endobronchial ultrasound-guided transbronchial needle aspiration, are recommended under local anesthesia to obtain tissue samples [
3]. However, in some instances, such when necrotic tissue accounts for a large proportion of the mass and it is difficult to obtain sufficient tissue for diagnosis, a surgical biopsy may be required. In our case study, tissue biopsy under local anesthesia failed due to the large proportion of necrotic tissue and a thoracoscopic excisional biopsy was the only remaining option. To prevent airway compromise, we planned to perform thoracic epidural anesthesia and maintain the patientŌĆÖs spontaneous respiration during surgery. Severe coughing and uncontrolled bleeding are the most common reasons for conversion to general anesthesia [
4]. Therefore, cough prevention was added by applying 4% lidocaine nebulization prior to surgery. As anesthetic management for non-intubated video-assisted thoracoscopic surgery (VATS) for mediastinal mass is rare, we report this case with specific emphasis on the anesthetic considerations.
CASE REPORT
A 22-year-old previously healthy male, suffering from a dry cough and dyspnea for 3-months, was scheduled for an anterior mediastinal mass biopsy. Symptoms included fatigue, fever, and weight loss (4 kg over 3 months). No wheezing was found on auscultation. The patient felt mildly dyspneic at rest and was most comfortable in a 45 degree position with his head elevated. A bulging mass was palpated on the left anterior neck region. CT scanning revealed a large anterior mediastinal mass compressing the mid-portion of the trachea, at the level of T2-4, which was deviated to the right side (
Fig. 1). CT images enabled measurement of the mass, which was approximately 13 ├Ś 10 cm and substantially larger than the narrowest part of the trachea (4.7 ├Ś 18.7 mm). A pulmonary function test (PFT) revealed a severe obstructive pattern with a peak expiratory flow (PEF) rate of 2.46 L/s (27% of the predicted value), forced expired volume per 1 s (FEV1) of 1.52 L (34% of the predicted value), and FEV1/forced vital capacity ratio (FEV1/FVC) of 31%. The patient felt discomfort when breathing in the supine position but, when sitting in a head-up position, pulse oximetry was above 97% and oxygenation was not required. Given that CT-guided percutaneous needle biopsy under local anesthesia and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) failed to obtain a sufficient tissue sample for diagnosis, a VATS biopsy was required.
Fig.┬Ā1
(A) Chest computed tomography image in the sagittal view, showing the large anterior mediastinal mass (both white arrows). (B) Chest computed tomography image in the transverse view, showing trachea deviation and narrowing due to the large mediastinal mass.

Thoracic epidural anesthesia was planned during VATS to prevent possible airway compromise during induction of general anesthesia. Thoracic epidural catheterization was performed at a pain medical center (Samsung Medical Center, Seoul, Korea) on the day of the surgery. With the patient in a prone position and under the guidance of fluoroscopy, a 19-guage epidural catheter (FlexTipPlus®, Arrow International, USA) was inserted into the T6-7 intervertebral space and the catheter tip was advanced up to T5. The position of the epidural catheter tip was confirmed by dispersion of a contrast medium. An epidural test dose of 3 ml was then performed, comprising 1.5% lidocaine and 15 μg epinephrine.
Two pieces of small-sized endotracheal tubes (internal diameter of 4.5 mm with cuff), a pediatric fiberoptic bronchoscope, and a number-4-sized supraglottic airway (i-gel
┬«, Intersurgical Ltd., United Kingdom) were prepared in the operating room for emergent conversion to general anesthesia. To ensure sufficient length, 2 small-sized endotracheal tubes were connected to each other using a sterile surgical tape. MurphyŌĆÖs eye on the connecting endotracheal tube was trimmed-off to ensure a wider and straighter tube at the join [
5]. As a precaution, the extracorporeal membrane oxygenation (ECMO) team was on stand-by during induction of anesthesia.
In the operating room, the patient was put into a 30-degree head-elevated position. The standard monitoring devices, including electrocardiography, pulse oximeter, and end-tidal carbon dioxide (ETCO2) were used. The patientŌĆÖs initial vital signs were stable; non-invasive blood pressure was 150/82 mmHg, heart rate was 98 beats/min with normal sinus rhythm, respiration rate was 15 breaths/min and pulse oximetry was 100%. Lidocaine nebulization (4 ml at 4% concentration; Nebulizer: PARI, Moosstrasse3, Germany) was administered for 15 min to suppress coughing. While the patient was on lidocaine nebulization, the radial artery was cannulated for invasive arterial blood pressure monitoring. Oxygen (5 L/min at 100% concentration) was administered via a facial mask, with an ETCO2 monitoring line attached to the mask during surgery.
Ropivacaine (15 ml at 0.75%; Ropivacaine HCl┬«, Hanlim pharm, Korea) mixed with fentanyl (1 ml of 50 ╬╝g) was administered for the thoracic blockade. A T3 to T10 sensory block was planned to enable multi-port surgery and chest tube insertion. Local anesthetic (3-4 ml) was administered incrementally through the epidural catheter after catheter aspiration. A dermatomal block was confirmed using warm-cold discrimination. Prepared local anesthetics (14 ml) were administered to reach the T3 sensory block within 15 min. A final check of the sensory block prior to surgery confirmed coverage from T2 to T11. After epidural anesthesia, the patientŌĆÖs vital signs were stable, with arterial blood pressure at 140/65-150/70 mmHg, heart rate at 85-90 beats/min with normal sinus rhythm, respiratory rate at 14-16 breaths/min, and pulse oximetry at 99-100%. No breathing difficulty was observed. After 20 min, the remaining 2 ml of prepared local anesthetic was administered through the epidural catheter to maintain anesthesia.
The uni-port method was chosen for the VATS biopsy, to decrease the patientŌĆÖs discomfort and achieve better control of collapse and inflation of the operated lung. The operation started with 4 cm of skin incision on the left 5th intercostal space, after sufficient skin and subcutaneous local tissue infiltration. The uni-port utility (4 cm, Glove port 4220-AS-3, Nelis medical, Korea) was then inserted and multiple tissue biopsies were performed (
Fig. 2).
Fig.┬Ā2
Uni-port utility scope view: mediastinal mass (white arrow) biopsy procedure.
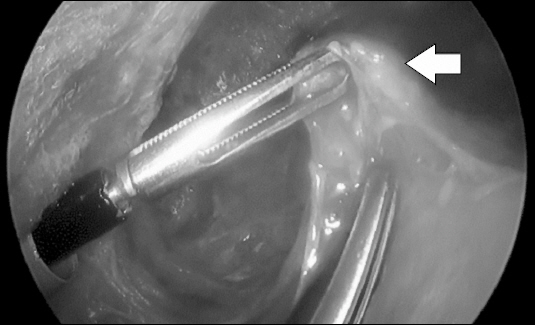
To minimize the possibility of respiratory compromise, the patient was not sedated during the surgery. The patient mentioned a slight discomfort, during the initial lung collapse, when the uni-port utility was introduced into the chest. However, it was temporary and the patient remained calm and comfortable throughout the procedure. Coughing was minimal and the patientŌĆÖs vital signs remained stable throughout the procedure; arterial blood pressure was 110/60 mmHg, heart rate was 78 beats/min with normal sinus rhythm, respiration rate was 15 breaths/min, and pulse oximetry was 100%.
After obtaining the frozen biopsy result and after bleeding control was achieved, a 12 Fr chest tube was inserted. The patient was transferred to the post anesthesia care unit without any complications.
The total operating time was 35 min. The anesthetic time was 63 min. A total of 250 ml of HartmannŌĆÖs solution was infused during the operation. Estimated blood loss was minimal and a urinary catheter was not required.
The large mediastinal mass was diagnosed as nodular sclerosis and classical HodgkinŌĆÖs lymphoma. The patient was discharged 6 days postoperatively, following his first cycle of chemotherapy, without problems.
DISCUSSION
In the current case, a VATS biopsy of a large anterior mediastinal mass was safely conducted by thoracic epidural anesthesia and lidocaine nebulization. Airway compression, due to a large mediastinal mass, can be fatal during general anesthesia; numerous case reports have described fatal or near-fatal cardiopulmonary arrest during anesthesia for diagnostic or therapeutic surgery in patients with a mediastinal mass [
2,
3,
6,
7]. Risk factors for respiratory compromise of a mediastinal mass include the patientŌĆÖs signs and symptoms, tracheal compression Ōēź 50%, mass volume Ōēź 130 cm
3, pleural effusion, pericardial effusion, superior vena cava compression, peak expiratory flow rate Ōēż 40% of the predicted value, and obstructive or mixed pulmonary dysfunction [
1,
5,
8]. Our patient presented with a palpable mass on his neck and showed dyspnea at rest. The mass measured 13 ├Ś 10 cm in diameter and compressed and deviated the trachea with severe obstructive PFT. Therefore, we anticipated airway collapse during general anesthesia and planned non-intubated VATS.
Recently, non-intubated VATS, a thoracoscopic technique without tracheal intubation, has grown in popularity given the potential to avoid intubation-related complications and thus expedite postoperative recovery [
4]. However, current reports on non-intubated VATS relate to the management of lung tumors, spontaneous pneumothorax, pleural effusions, empyema and emphysema, as well as lung volume reduction surgeries and lung biopsies for interstitial lung disease [
4,
8-
11]. The use of non-intubated VATS for large mediastinal mass biopsies is currently underreported. Our case indicates that non-intubated VATS can be conducted for the biopsy of a large mediastinal mass.
Several anesthetic methods can be employed for non- intubated VATS. Local anesthesia under monitored anesthesia care for non-intubated VATS was successfully performed in previous reports [
11,
12]. However, it can be challenging to control the exact level of sedation and analgesia to meet both the requirements of the surgeon and patient, whilst also maintaining adequate respiration. Moreover, use of non- intubated VATS is also only appropriate for simple biopsies around peripherally located lesions. Intercostal nerve block can be used for non-intubated VATS, and is associated with relatively minor patient discomfort and pain; however, obtaining an adequate blockade of the thoracic region may be complex and the block duration may be limited. Moreover, complications, such as pneumothorax, may occur as well as instances of local anesthetic systemic toxicity [
11,
12]. An alternative method for non-intubated VATS includes epidural catheter insertion, which has several advantages over the previously mentioned approaches, including potential for additional local anesthetic injection during operation, increased anesthetic duration, and the potential provision of postoperative analgesia, where required. Furthermore, epidural block increases myocardial blood flow and reduces myocardial oxygen consumption, which is advantageous for cardiorespiratory compromised patients [
8,
9]. However, epidural anesthesia may cause systemic hypotension and is contraindicated in patients receiving anticoagulation therapy.
There are some anesthetic considerations for non-intubated VATS. Firstly, VATS requires a well deflated lung, and incomplete cough prevention can lead to surgery termination and vascular or tissue injury. In our case, 4% lidocaine nebulization was sufficient for cough prevention. For additional cough prevention, vagus nerve block, phrenic nerve block, and infiltration of local anesthetics into pleura have been performed, and these additional measures may be necessary for more invasive procedures, such as lobectomy [
12,
13]. Secondly, urgent conversion to general anesthesia may have catastrophic results. Again, severe uncontrollable coughing is the most common cause of conversion to general anesthesia, but other causes include persistent hypoxemia, surgical difficulty, ineffective analgesia, bleeding, change of surgical plan, and an anxiety attack [
4,
10,
11,
14,
15]. Despite extensive planning and caution, urgent conversion to general anesthesia is sometimes necessary and thus emergency preparation for should always be undertaken. Intubation is usually performed in the lateral position. Before emergency intubation, the operation should be stopped, the chest tube inserted, the surgical wound sealed with sterile adhesive tape, and the lung inflated with mask ventilation. In these situations, a video-laryngoscopy or fiber- optic bronchoscopy is useful for faster and easier intubation in a lateral decubitus position. An endobronchial blocker or long endotracheal tube can be used for lung separation. We prepared an airway device including a supra-glottic airway (small plain tubes, connected to ensure sufficient length), and an ECMO team was on stand-by during induction.
In conclusion, a surgical excisional biopsy for a large mediastinal mass was successfully performed by means of a non-intubated VATS in our patient. Thoracic epidural anesthesia combined with lidocaine nebulization seems to be safe and sufficient for patients with anticipated airway compromise undergoing VATS.





