Hemodynamic response to tracheal intubation and postoperative pharyngeal morbidity using GlideScope®, Lightwand and Macintosh laryngoscopes during remifentanil infusion
Article information
Abstract
Background:
Use of GlideScope® laryngoscopes and lightwands for tracheal intubation does not require much force. Theoretically, less stimulation can reduce hemodynamic changes during intubation. We investigated the hemodynamic response to tracheal intubation using different laryngoscope types during remifentanil infusion.
Methods:
Sixty American Society of Anesthesiologists class I-II patients were compared in terms of tracheal intubation time, hemodynamic changes, and postoperative pharyngeal complications when using a GlideScope®, lightwand, or Macintosh laryngoscope. Propofol and rocuronium were injected and remifentanil was infused for three minutes. Blood pressure and heart rate were measured before and 1, 3, and 5 minutes after tracheal intubation. Patients were assessed for postoperative oral and tracheal bleeding as well as hoarseness, dysphagia, and sore throat.
Results:
Intubation time was prolonged in the GlideScope® group. All three groups showed a significant decrease in systolic and diastolic blood pressure 1, 3, and 5 minutes after tracheal intubation. Heart rates increased significantly in all three groups immediately after intubation as well as 1 minute later in the GlideScope® group. However, there were no differences in blood pressure, heart rate, or the occurrence of hoarseness, dysphagia, and sore throat among the three groups.
Conclusions:
No differences in hemodynamic change were found among the three different techniques.
INTRODUCTION
Traditional tracheal intubation uses a direct laryngoscope to expose the vocal cords and insert a tracheal tube with visual confirmation. However, if the vocal cords are not easily exposed, excessive force must be applied during tracheal intubation, which can affect sensory receptors of the larynx and pharynx. This can cause increases in blood pressure and heart rate due to hemodynamic stress [1-4] and may lead to adverse cardiovascular events [5]. Damage to surrounding tissue may result in hoarseness, dysphagia, and sore throat after extubation. Difficult tracheal intubation may cause serious damage to the soft tissue of the upper airway, prompting a rise in blood pressure and complications such as stroke [6, 7]. If intubation fails and the airway is not secured, patient morbidity and mortality increases.
A direct Macintosh laryngoscope is commonly used for tracheal intubation. Recently, new laryngoscopes have been developed that do not require oral, pharyngeal, and tracheal axis alignment, allowing for clearer exposure of the vocal cords. The Glidescope® (Saturn Biomedical System Inc., Canada) has a light source and digital camera attached to the end of the laryngoscope blade. It provides a view of the vocal cords on a 7” LCD monitor. Its blade is angled at 60°, so it does not require much force around the vallecula to expose the vocal cords compared to a direct laryngoscope.
The lightwand has a light source at the tip of a stylet. As the end of the lightwand enters the trachea through the vocal cord, the light shines toward the front of the neck, indicating that intubation was successful. Since the use of the lightwand for intubation does not involve direct observation of the vocal cord, it is less invasive than traditional direct laryngoscope intubation.
This study compared systolic blood pressure (SBP), diastolic blood pressure (DBP) and heart rates as well as postoperative hoarseness, dysphagia, and sore throat among three groups (GlideScope®, lightwand, or Macintosh laryngoscope) during intubation with remifentanil infusion.
MATERIALS AND METHODS
The study was approved by the Ethical Committee of our hospital and the patients. Sixty patients aged 20–60 years with an American Society of Anesthesiologists (ASA) physical status of I or II were enrolled. All data were collected by a fourth-year resident doctor. Patients were randomized to intubation with either GlideScope®, lightwand, or Macintosh laryngoscope (size 3 blade). All intubations were performed by an experienced anesthesiologist who had handled each device more than 30 times.
The following patients were excluded: those with a history of hypertension, airway lesion, perioperative sore throat, and body mass index > 30 and those with more than two of the following four criteria: thyromental distance less than 6 cm, Mallampati classification of III/IV, inter-incisor distance less than 4 cm, and cervical spine immobilization.
Standard monitoring, such as Electrocardiography, non-invasive arterial blood pressure, and pulse oximetry were applied before induction of anesthesia. Pre-oxygenation was performed with 100% oxygen for two minutes, remifentanil was infused at a rate of 0.15 μg/kg/min with normal saline 300 ml/h, and propofol (2 mg/kg) was injected intravenously to initiate loss of consciousness. Manual ventilation using 2.0% sevoflurane with oxygen was performed in all patients. After proper mask ventilation was performed, 0.8 mg/kg of rocuronium was injected. Three minutes after the injection of rocuronium, intubation was performed using one of the three laryngoscope devices. Anesthesia was maintained with 50% oxygen in air, 2 vol% sevoflurane, and remifentanil infusion of 0.15 μg/kg/min for 5 minutes. Respiratory volume was maintained at 10 ml/kg, respiratory rate was maintained at 10–12 breaths/min, and end tidal CO2 was maintained between 35 and 40 mmHg. We measured the baseline, pre-intubation, immediately after intubation and post-intubation (1, 3, and 5 minutes) SBP, DBP and heart rate. Duration of intubation time, number of attempts for successful intubation, and whether external laryngeal pressure was applied were recorded. Cases requiring more than three attempts or a duration of longer than 60 seconds were defined as failure. Intubation time was from the moment the device was inserted into the patient’s mouth until it was removed from the mouth. If tracheal intubation failed, the patient was excluded from the study and the case was managed according to difficult airway algorithms and ASA guidelines. In female patients, 7.0 mm (ID) tubes were used and 8.0 mm (ID) tubes were used in male patients. In the GlideScope® group, the tracheal tube was prepared according to the manufacturer’s pre-configured stylet. In the lightwand group, the tracheal tube end was pre-loaded at a 90° angle. Thirty minutes after the end of the operation, of the presence or absence of mucosal bleeding, hoarseness, dysphagia, and sore throat were recorded. Grade of sorethroat, hoarseness, and dysphagia were evaluated using 4-point verbal rating scales as follows [8]: hoarseness 0 = absent, 1 = slight, 2 = severe, 3 = cannot speak because of hoarseness; dysphagia 0 = absent, 1 = slight, 2 = severe, 3 = cannot swallow because of dysphagia; sore throat 0 = absent, 1 = minimal, 2 = moderate, 3 = severe sore throat.
Based on a previous study [9], a sample size of 20 patients per group was required to achieve 80% power at a 5% significance level. To compare differences among the three groups, we assessed heart rate and SBP. Continuous variables were expressed as mean ± standard deviation; categorical variables were presented as frequency and ratio. Continuous variables were compared using ANOVA (time to successful intubation, systolic and diastolic blood pressure, heart rate, thyromental distance, interincisor distance), while categorical variables were compared using the Pearson chi-square test. The level of significance was a P value < 0.05. ANOVA was used to compare time to successful intubation and hemodynamic changes. All analyses were performed using SAS version 9.4 (SAS Inc., USA).
RESULTS
There were no significant differences among patients in the three groups except intubation time (Table 1). Intubation time was significantly longer in the GlideScope® group than in the other two groups (P < 0.05) (Table 1). A duration of intubation longer than 60 seconds was considered a failure; there was one failed case in the lightwand group and one in the GlideScope® group. External laryngeal pressure was applied once in the Macintosh group, while none was required in the lightwand or GlideScope® group. Mucosal bleeding was found in two patients in the lightwand group, four patients in the GlideScope® group, and three patients in the Macintosh group. There were no differences in the occurrence of sore throat, hoarseness, and dysphagia among the groups (Table 1). In all three groups, SBP and DBP decreased below baseline blood pressure before intubation and 1, 3, and 5 minutes after tracheal intubation (P < 0.05) (Figs. 1 and 2). Immediately after intubation, SBP and DBP showed baseline values, and there were no differences among the three groups (Figs. 1 and 2). Heart rate increased in all three groups after intubation, but recovered to baseline within one minute, except in the GlideScope® group (P < 0.05) (Fig. 3).

Comparison of systolic blood pressure (SBP) changes. All values are expressed as mean ± SD. BL = baseline, BI = before intubation, AI = immediately after intubation. T1–T5 = points of time as minutes after intubation. †Compared with baseline values in GlideScope® group. *Compared with baseline values in Lightwand group. ‡Compared with baseline values in Macintosh group. *,†,‡P < 0.05 compared with baseline values.
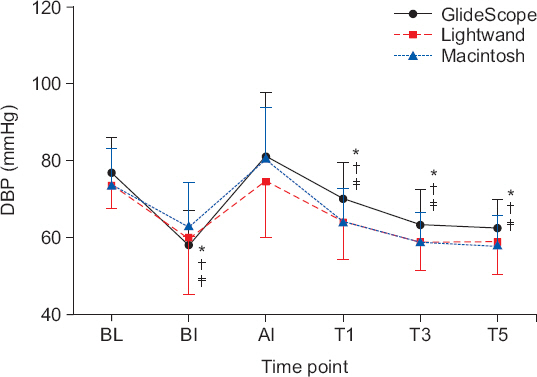
Comparison of diastolic blood pressure (DBP) changes. All values are expressed as mean ± SD. BL = baseline, BI = before intubation, AI = immediately after intubation. T1–T5 = points of time as minutes after intubation. †Compared with baseline values in GlideScope® group. *Compared with baseline values in Lightwand group. ‡Compared with baseline values in Macintosh group. *,†,‡P < 0.05 compared with baseline values.

Comparison of heart rate (HR) changes. All values are expressed as mean ± SD. BL = baseline, BI = before intubation, AI = immediately after intubation. T1–T5 = points of time as minutes after intubation. †Compared with baseline values in GlideScope® group. *Compared with baseline values in Lightwand group. ‡Compared with baseline values in Macintosh group. *,†,‡P < 0.05 compared with baseline values.
DISCUSSION
Orotracheal intubation using a laryngoscope uses a blade to raise the glottis 45° degrees upward, causing hemodynamic changes [1-3]. Therefore, to alleviate hemodynamic changes caused by tracheal intubation, careful manipulation of the laryngoscope to decrease supraglottis stimulation is important. Still, sore throat and dysphagia may result from glottis stimulation, and using a lightwand rather than a rigid laryngoscope decreased the incidence of these post-operative symptoms [9-11].
In this study, all three laryngoscope techniques were expected to allow easy tracheal intubation. However, there were differences in intubating time; more time was required to perform intubation in the Glidescope group compared to the other two groups. Patients involved in the study had normal anatomical structures, so the use of a Macintosh laryngoscope or lightwand by an experienced anesthesiologist should not have been problematic. Also, SBP and DBP before intubation and 1, 3, and 5 minutes after intubation decreased significantly compared to the baseline blood pressure. However, SBP and DBP immediately after intubation were similar to the baseline blood pressure. There were no differences in cardiovascular responses among the three groups following tracheal intubation. This could be the result of appropriate remifentanil infusion, which likely decreased response to stimulation.
In normotensive patients, compared to the use of the Macintosh laryngoscope, an airway scope caused less hemodynamic changes [12]. This is because manipulation of the airway scope causes less glottal stimulation than the Macintosh device. To decrease hemodynamic changes during tracheal intubation, fentanyl or remifentanil may be injected before the procedure [13]. Nishikawa et al. [14] reported that in normotensive patients, intubation with the lightwand took longer than the laryngoscope, but hemodynamic changes after tracheal intubation were less profound. This study showed different results than previous studies, which suggested that hemodynamic changes after intubation were not affected by different devices. This may be due to the fact that the lightwand technique does not require a large mouth opening or lifting of the epiglottis [15].
Use of video laryngoscopy is advantageous because it allows better visualization of the glottis entrance. However, it does not guarantee easier or successful tracheal tube insertion. Among video laryngoscopes, the airway scope shortens intubation time [16]. It is also easier to use than other laryngoscopes such as the GlideScope®, C-MAC, or Macintosh. This is because the tracheal tube is attached to the airway scope and following the airway scope guidance system allows for easier and quicker intubation. The Cormack and Lehane classification type I ratio was higher in the GlideScope® group (78%) than in the Macintosh group (58%), but the ratio of multiple attempts and postoperative sore throats was higher in the GlideScope® intubation group [12]. Also, they reported that the percentage of patients with Cormack & Lehane grade I was higher in the GlideScope® group than in the Macintosh group.
Depending on the degree of difficulty in intubation, there was a difference between hemodynamic changes and intubation time among the groups. Lim et al. [17] reported that in patients who are easy to intubate, use of the Macintosh laryngoscope took less time than use of the GlideScope®. However, in difficult intubation cases, intubation time was much faster in the GlideScope® group. In our study, intubation via the Macintosh device in patients with a Mallampati score of I or II was much faster than using the GlideScope®. Short intubation time and minimal occurrence of complications such as hoarseness, sore throat, and dysphagia in the lightwand group resulted in less glottis stimulation when performed by an experienced anesthesiologist. If lightwand intubation was performed by an anesthesiologist unfamiliar with the lightwand, the results may have been different.
There have been reports that injection of fentanyl before intubation decreases hemodynamic changes [2,18,19]. In the Macintosh group, supraglottic stimulation may greatly affect hemodynamics; however, there were no differences blood pressure changes after intubation among the three groups in our results. We believe that the use of remifentanil decreased hemodynamic changes in all three groups. Thus, appropriate use of remifentanil is more important than reducing supraglottic stimulation in the alleviation of hemodynamic changes during tracheal intubation. Also, β-adrenergic antagonist esmolol and lidocaine are used for the prevention or treatment for unwanted perioperative hemodynamic responses during intubation [20,21].
There are several limitations to our study. First, the study consisted of patients with normal blood pressures and airways. Therefore, there may have been differences in intubation time among the three groups if patients were difficult to intubate. Also, as shown in Koyama’s study [12], normotensive patients and hypertensive patients show variable hemodynamic change. Secondly, we only checked for postoperative complications in the recovery room thirty minutes after the surgery had ended. We were not able to evaluate whether patients experienced symptoms outside of the recovery room. Third, we chose patients randomly, but did not select them using double blinding, so selection may have been prone to bias. Furthermore, we considered patients in the lightwand and GlideScope® groups whose intubation time took more than one minute as failures and excluded them from the study. We did not take into consideration the hemodynamic changes in patients requiring either multiple attempts or prolonged intubation time. Finally, use of remifentanil had a greater effect in alleviating glottal stimulation; instead of hemodynamic changes being caused by different devices, use of remifentanil might have had an influence.
In conclusion, use of GlideScope®, lightwand, or Macintosh laryngoscope enables rapid tracheal intubation. In this study, there were no differences in hemodynamic changes among the three methods of intubation.
