Guidewire insertion into the vertebral vein during right internal jugular vein central venous catheterization -A rare case report-
Article information
Abstract
Background
Internal jugular veins are the most frequently accessed site for central venous catheterization in patient management, whereas complications involving vertebral veins are a rare occurrence.
Case
A 73-year-old male suspected to have a urothelial carcinoma was scheduled for elective left nephroureterectomy. During central venous catheterization using the anatomic landmark technique to target the internal jugular vein, a guidewire is inadvertently inserted into the suspected vertebral vein. Following the correction of the catheterization, a radiologist reviewed the preoperative enhanced computed tomography and confirmed that the initially punctured vessel was the vertebral vein. On the third day after surgery, the central venous catheter was removed, and the patient did not exhibit any complications, such as bleeding, swelling, and neurological symptoms.
Conclusions
The use of ultrasonography during central venous catheterization is recommended to evaluate the anatomy of the puncture site and prevent misinsertion of the catheter, which can lead to several complications.
As practitioners of anesthesiology and pain medicine, we have frequently been required to access numerous veins; among the tools used to access these veins, the central venous catheter is a powerful and essential tool in patient management. Despite various benefits, central venous catheterization, especially when targeting the internal jugular vein, can lead to significant complications, such as common carotid artery puncture, pneumothorax, hematoma, arteriovenous fistula formation, venous infarction, catheter entrapment, and fluid leakage [1,2]. During surgical procedures, the internal jugular vein is the most frequently accessed site for central venous catheterization in patient management, whereas complications involving the vertebral vein are a rare occurrence. In this case report, we describe the insertion of a guidewire into the vertebral vein during an attempted central venous catheterization targeting the internal jugular vein.
CASE REPORT
A 73-year-old male (174 cm, 47 kg) with the American Society of Anesthesiologist physical classification of 3 was scheduled for elective left nephroureterectomy. A left calyx tumor was incidentally discovered during a routine medical examination, and a biopsy performed 1 month ago during ureteroscopy suggested a urothelial carcinoma. Past medical history includes intraductal papillary mucinous neoplasm of the liver that was surgically removed 6 years ago. A preoperative evaluation was performed, and chest computed tomography (CT) revealed pulmonary thromboembolism in the left lower lobe. A lower extremity ultrasonogram showed no evidence of deep vein thrombosis, and arterial blood gas analysis and D-dimer were within the normal ranges. The patient was instructed to fast for 8 hours (nothing by mouth) before undergoing general anesthesia. Premedication involved administrating an intramuscular injection of glycopyrrolate (0.2 mg) and famotidine (20 mg). In the operating room, noninvasive monitoring devices were placed on the patient, including a blood pressure cuff, electrocardiogram, a pulse oximeter, a bispectral index signal device, and a quantitative monitor for neuromuscular blockade. General anesthesia was induced using 80 mg propofol, followed by 30 mg rocuronium for neuromuscular blockade after confirming no response to stimuli. Then, sevoflurane (1.7%) was used to maintain the appropriate anesthesia depth after intubation. Because of the risk of bleeding from renal artery surgery, an arterial line was inserted into the right radial artery. Furthermore, right internal jugular vein central venous catheterization was planned. Real-time ultrasound-guided catheterization was initially planned; however, the hospital’s portable ultrasonography device was in use in other operating rooms; therefore, a blind catheterization technique was used based on the patient’s anatomical structure without ultrasound guidance. The patient was positioned in the Trendelenburg position with the head 15° below the horizontal plane and tilted 40° to the left. The Bermuda triangle, an anatomical structure formed by the posterior margin of the sternal muscle belly of the sternocleidomastoid muscle, the anterior margin of the clavicular muscle belly, and the upper margin of the clavicle, was clearly identified. The carotid artery pulse was palpated at the superior angle of the triangle and followed to the center of the triangle, where a 10 ml syringe connected to a 23-gauge finder needle was inserted perpendicularly to the surface while aspirating. The presence of dark venous blood was confirmed at a depth of 2.2 cm, and no pulsation was observed after separating the finder needle from the syringe. Then, the 18-gauge puncture needle connected to the syringe was inserted toward the nipple at a 75° angle from the skin while targeting the finder needle tip, and the aspiration of venous blood flow was confirmed. After removing the finder needle, a guidewire was inserted to a depth of 20 cm from the skin through the puncture needle without any resistance felt during the procedure. The puncture needle was removed while leaving the guidewire in place. Prior to inserting the dilator, the practitioner and colleagues, experiencing a sense of unease during the procedure, attempted to investigate the anatomy of the puncture site by utilizing ultrasonography to detect the previously inserted guide wire, prompted by their concern that the depth of the finder needle, measuring 2.2 cm, is deeper than observed in other patients, which contributed to their uneasiness. The guidewire was found to be located in a vein as which we presumed the vessel based on its location that was lateral from the common carotid artery and collapsibility when pressure was applied using the probe. However, a larger vessel presumed to be a vein was located superiorly and more laterally than the identified vessel. Real-time ultrasound-guided guidewire insertion was performed at the same view in this vessel using another central venous catheter kit. Both guidewires were left in place while the probe was tilted to visualize their paths, and it was confirmed that they were both descending toward the right brachiocephalic vein (Fig. 1). The first guidewire was removed, and manual compression using sterile gauze was applied for over 5 min. No resistance was felt during the removal. The second guidewire was used to complete the central venous catheterization, and free regurgitation was observed at each port. The central venous pressure (CVP) measured using the central venous catheter was 15 mmHg. The surgery was successful, and the patient was transferred to the post-anesthesia care unit after extubation. A simple anterior-to-posterior chest X-ray (CXR) taken immediately after the surgery confirmed that the catheter tip was located near the right atrium, following the superior vena cava (SVC) (Fig. 2). We reviewed the contrast-enhanced chest CT performed for preoperative evaluation and confirmed that the right internal jugular vein coursed laterally to the right common carotid artery on the axial view. A large vessel was also observed behind the common carotid artery and internal jugular vein, and it was traced upward and downward, confirming that it enters into the transverse foramen at the level of the sixth cervical vertebra and drains into the right brachiocephalic vein, consistent with the known course of the cervical vertebral vein. The same findings were observed in the coronary view (Fig. 3). The radiologist indicated this vessel as the vertebral vein. After considering the ultrasonographic findings and the radiologist’s official reading, we confirmed that the vein that we had initially punctured was indeed the right cervical vertebral vein. On the third day after surgery, the central venous catheter was removed, and the patient did not exhibit any complications, such as bleeding, swelling, and neurological symptoms.
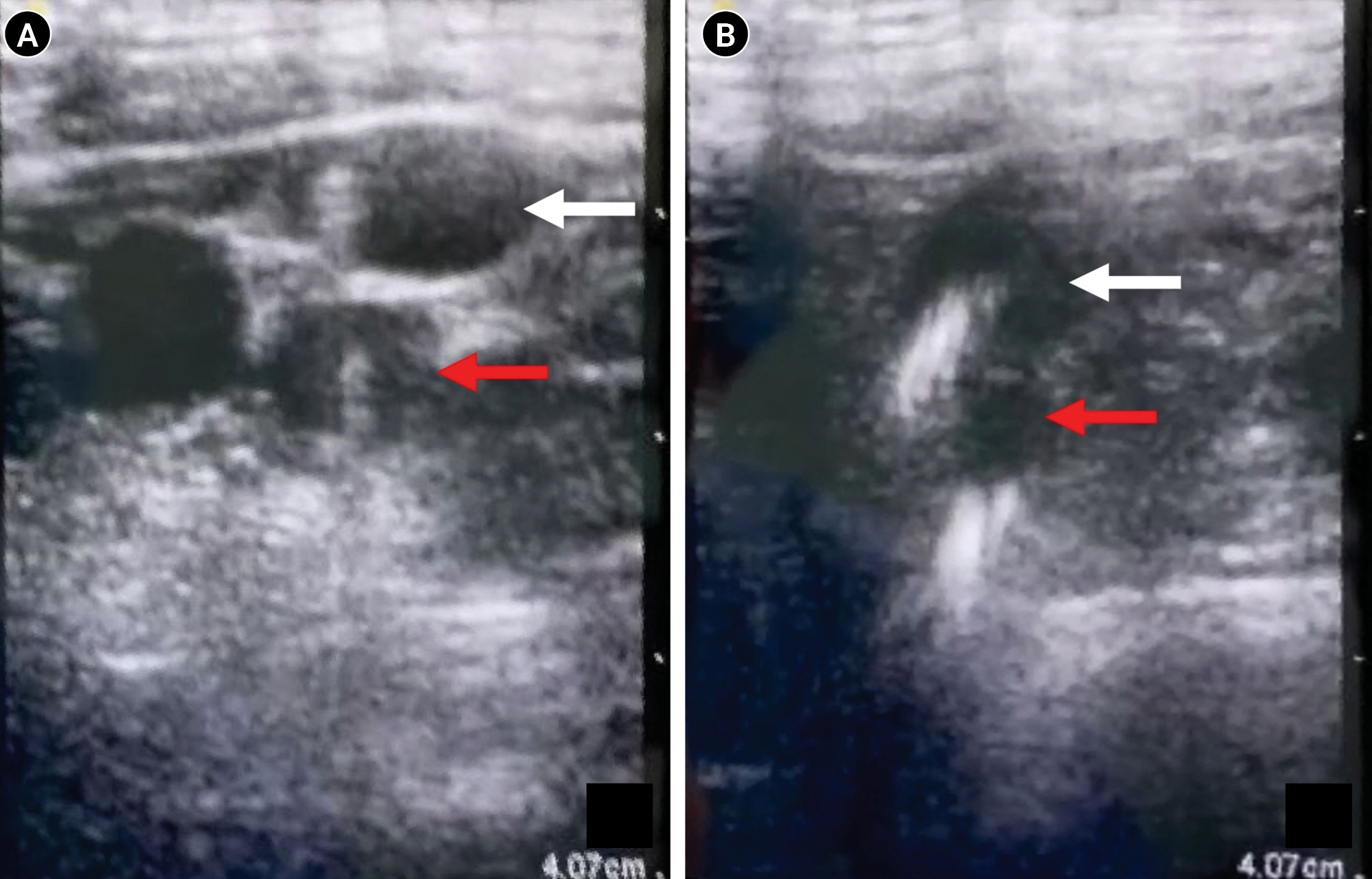
Ultrasonography. (A) A larger vessel where the second guidewire was inserted is located superiorly and more laterally than the vessel that was first punctured. (B) The course of both veins, where the guidewires were inserted, descends toward the right brachiocephalic vein. Red arrow: vertebral vein; white arrow: internal jugular vein.
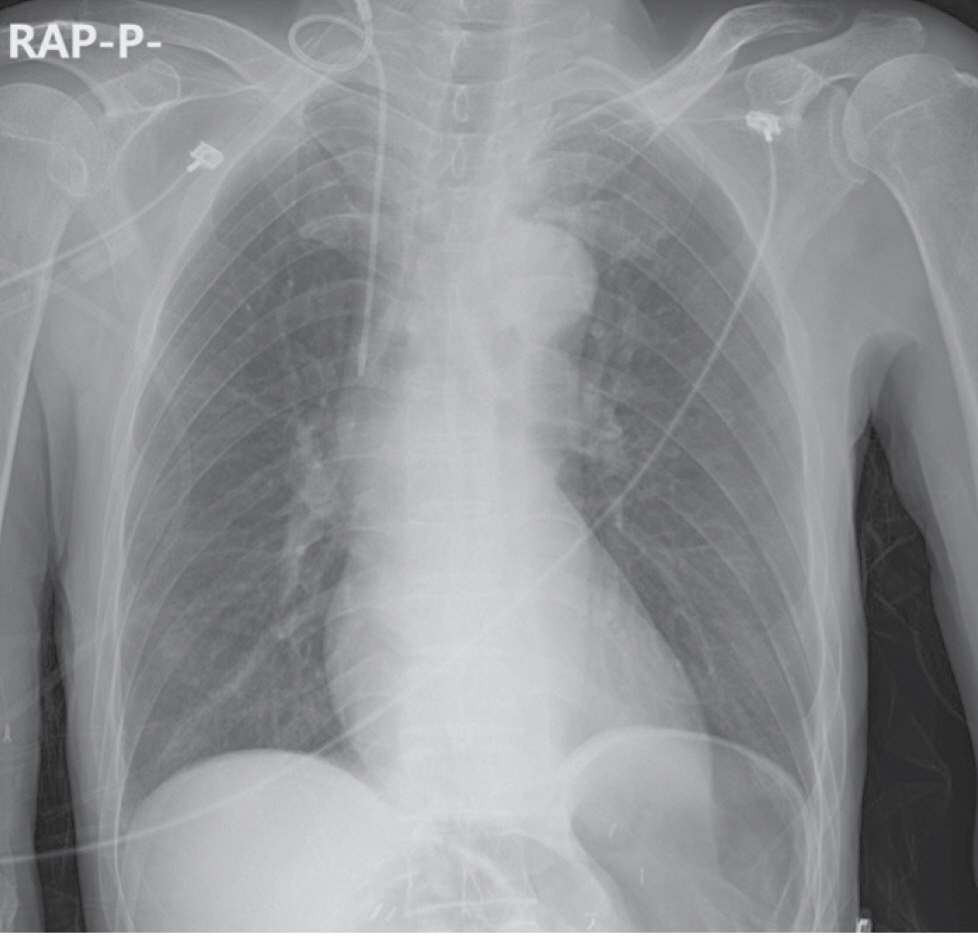
The central venous catheter, which was cannulated using the second inserted guidewire, is located near the right atrium and follows the superior vena cava.

Contrast-enhanced computed tomogram. (A) The axial view at the seventh cervical vertebral level reveals a suspected vein running from the vertebral foramen of the sixth cervical vertebra. (B) Coronary view of the same computed tomogram also reveals an escape of the suspected vein from the sixth vertebral foramen. Red arrow: suspected vein.
DISCUSSION
Every year, more than 5 million cases of central venous catheter insertion are performed by clinicians, with various purposes, particularly in anesthesiology and pain medicine, where a greater number of central venous catheter insertions are performed after anesthesia induction to control the patient’s condition during surgery, such as the use of inotropes and vasopressors, volume resuscitation, and CVP monitoring for fluid management [3,4]. The internal jugular vein is the most commonly used site for central venous catheter insertion because of its superficial location compared with other large veins, ease of confirmation with ultrasound, and direct connection to the SVC in the case of the right internal jugular vein [3]. Furthermore, except for surgeries of the head and neck, most surgeries allow for easy access to the insertion site for anesthesiologists. However, approximately 15% of central venous catheterization cases result in complications, such as arterial puncture, pneumothorax, vessel erosion, thrombosis, occlusion, airway obstruction, malposition of the catheter tip, and delayed infection, with arterial puncture being the most common complication [1,3]. The malposition of the catheter tip occurs relatively commonly, at a rate of 5.01% [2].
Various veins are located near the internal jugular vein, including the external jugular vein, anterior jugular vein, subclavian vein, mammary vein, accessory hemiazygos vein, and vertebral vein. Among these, the vertebral vein is a very small vessel located behind the internal jugular vein, passing through the transverse foramen from the atlas to the sixth cervical vertebra and drains into the brachiocephalic vein. Due to its relatively small size and deep course compared with the internal jugular vein, inadvertent catheterization of the vertebral vein during central venous access is a rare occurrence. However, there are a few case reports where this occurrence happened [1,2,4,5].
In this case, we attempted a blind central venous catheterization using anatomical landmarks, considering the characteristics of the patient and the surgery. During the insertion procedure, we realized that the depth of the finder needle was deeper than usual, and we confirmed the location of the guidewire using ultrasound. After confirming that the first inserted guidewire was located in a vein deeper than the common carotid artery, we performed real-time ultrasound-guided central venous catheterization on the vessel expected to be the internal jugular vein and safely removed the original guidewire. A CXR performed after the procedure confirmed that the inserted central venous catheter was appropriately placed in the SVC. The radiologist indicated the first punctured vein as the vertebral vein with enhanced CT after surgery.
The cause of vertebral vein puncture is thought to be mainly due to the excessive rotation of the patient’s head. When the head rotates more than 30°, the internal jugular vein overlies the common carotid artery, increasing the likelihood of inadvertent puncture of the vertebral vein, which is beneath the internal jugular vein [5]. In a previous case of vertebral vein cannulation, the patient’s head was rotated approximately 50° to the left [5]. In our case, the patient’s head was rotated 40° to the left for central venous catheterization. However, ultrasound after the insertion of the first guidewire showed that the position of the internal jugular vein did not overlap with the common carotid artery; therefore, the vertebral vein puncture in this patient was difficult to be attributed to excessive head rotation.
Another cause is the deep insertion of the finder needle. The internal jugular vein is typically located 1.0-1.5 cm deep from the skin surface, and when the needle is inserted at an angle of 30°, it barely exceeds 3.5 cm from the skin surface to the internal jugular vein [3,5]. If it is inserted deeper than this, the pressure from the needle can cause the collapse of the internal jugular vein, leading to puncture of the posterior wall of the internal jugular vein and the vertebral vein. In a previous case report, when a finder needle was inserted at a 30° angle to a patient with a body mass index of 30 kg/m², venous blood was aspirated at a depth of 4 cm, and the vessel was predicted to be the vertebral vein [5]. In our case, the finder needle was inserted perpendicularly from the surface, at a depth of 2.2 cm. This depth corresponds to a depth of 4.4 cm if the needle had been inserted at a 30° angle. In addition, the patient was underweight with a body mass index of 15.5 kg/m²; therefore, the distance from the skin to the internal jugular vein was expected to be shallower than that in the previous case. Therefore, the depth of the finder needle insertion in our case was quite deep and sufficient to puncture the vertebral vein.
The angle at which the puncture needle is inserted also be considered as a potential reason for the puncture of the vertebral vein. A study conducted by Kobayasi et al. [6] showed an optimal angle and velocity of inserting a puncture needle in terms of safe catheterization. For a safe catheterization, it is important to ensure that the tip of the puncture needle is positioned within the target vein to avoid accidental puncture of structures located below the internal jugular vein. The study investigated two physical indices for evaluating the ease of stopping a needle inside a vein. These indices included the magnitude of the sudden decrease in reaction force when the needle advances into the vein and the duration for which the needle tip remains inside the vein. A larger decrease in reaction force indicates that the practitioner can more easily perceive when the superior wall of the vein is pierced. Similarly, a longer duration of the needle tip within the vein suggests a lower likelihood of penetrating through both walls of the vein. Based on these factors, it is recommended to insert the puncture needle at an angle of 10-20°, with a velocity of 3 mm/s, which minimizes tissue deformation because of tissue viscoelastic properties [6,7]. In comparison, the insertion angle of 75° in this case is much steeper and could lead to complications by penetrating both walls of the vein. However, if the initial puncture needle reached the vertebral vein through the internal jugular vein, the pathway of the guide wire, inadvertently inserted into the vertebral vein, should also involve the internal jugular vein. The subsequent examination with an ultrasonogram confirmed that both guide wires ran independently, providing no evidence of the guide wire passing through the internal jugular vein. This suggests that although the 75° insertion angle of the puncture needle was relatively steep in terms of safe catheterization, it was not the cause of the puncture of the vertebral vein in our patient.
In this case, it is expected that the probability of vertebral vein puncture would be increased because the right vertebral vein of the patient was more engorged than that of the general population. According to a study by Ciuti et al. [8], the mean area of the right vertebral vein in the supine position for 25 healthy volunteers with a mean age of 27 years was 2 ± 1 mm2 (mean ± standard deviation), whereas the mean area of the left vertebral vein was 6 ± 25 mm2, which is larger than the right one. The mean area of the right and left internal jugular vein was 42 ± 40 mm2 and 41 ± 25 mm2, respectively.
Our patient’s cross-sectional area of the right vertebral vein at the preforaminal (V1) segment, calculated using the axial view of the enhanced chest CT performed before the surgery, was 42.2 mm2 (left vertebral vein; 11.7 mm2, right internal jugular vein; 49.8 mm2, left internal jugular vein; 40.6 mm2), which is approximately 21 times larger than the mean area of the right vertebral vein in the general population [8]. Moreover, at the same level, it is approximately 3.6 times larger than the area of the opposite vertebral vein. During the central venous catheterization procedure, ultrasonography confirmed that there was no significant difference in the cross-sectional area between the internal jugular and vertebral veins.
Although the reason for the enlargement of the patient’s right vertebral vein was uncertain, it is speculated that the previous left hemihepatectomy, caudate lobe (S1) segmentectomy, and bile duct resection may have affected the systemic venous return by causing the enlargement of the intrahepatic duct and hepatic vein. This is supported by the fact that the CVP measured in the supine position after the central venous catheter insertion was 15 mmHg.
Catheterization through the vertebral vein also leads to various complications, including hematoma, arteriovenous fistula formation, venous infarction, catheter entrapment, and fluid leakage, similar to those of internal jugular vein catheterization [1,2]. Furthermore, a case study by Winston et al. [9] reported brachial plexopathy resulting from the migration of chemotherapeutic agents through a catheter that was inserted into the vertebral vein. In the most recent case, vocal cord palsy occurred 2 days after catheterization of the left vertebral vein, and the symptoms resolved after the removal of the catheter [10]. During catheter removal, hematoma and vein tears are possible complications. Because of the vertebral vein’s course through the transverse foramen of the cervical vertebra, external compression may not be sufficient to control bleeding, and radiological intervention or surgical exploration may be necessary. Therefore, it is recommended that catheter removal should be performed in a prepared hybrid operating room [1].
Central venous catheter placement is typically confirmed using a simple CXR. However, one of the drawbacks of using a simple CXR is that it cannot be used as a preventative measure to confirm the position of the catheter before insertion. While the use of portable X-ray or C-arm equipment within the operating room can be used to confirm the position of the guidewire before insertion, there are limitations to their availability and time constraints when using these tools for all central venous catheterizations. Ultrasonography is a useful tool that not only allows for the easy confirmation of the puncture site anatomy but also provides real-time in plane and out-of-plane views to identify the needle’s position during the procedure. In our case, although the initial guidewire insertion was achieved using the landmark technique, the use of ultrasonography prevented vertebral vein catheterization and allowed for the appropriate insertion of the central venous catheter within the internal jugular vein. This case emphasizes the importance of using ultrasonography as a necessary tool rather than a choice in central venous catheterization procedures.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Jeonghan Lee, Jaewoo Suh, Juseok Oh, Seunghee Ki. Writing - original draft: Jaewoo Suh. Writing - review & editing: Jaewoo Suh, Juseok Oh, Seunghee Ki. Supervision: Jeonghan Lee, Seunghee Ki.
