|
 |
- Search
| Anesth Pain Med > Volume 18(1); 2023 > Article |
|
Abstract
Background
Changes in tissue oxygen saturation determined by near-infrared spectroscopy (NIRS) may help predict and determine the success of a lateral infraclavicular (LIC) block. We investigated whether evaluation of tissue oxygen saturation determined by NIRS could be an indicator of LIC block success.
Methods
Forty patients scheduled for hand or forearm surgery under LIC block were studied. NIRS sensors were placed on the ventral aspect of both mid-forearms, and the contralateral hand was used as the control group. NIRS values were recorded before the block and at regular intervals during the following 30 min.
Results
NIRS values were significantly higher in the successfully blocked patients when compared to the complete failure, partial failure, and contralateral hand groups at the 10th min. In the successfully blocked patients, NIRS values (mean ± SD [change in %]) increased by 11.09 ± 4.86 (16.03%), 15.00 ± 4.53 (21.76%), 16.35 ± 5.14 (23.77%), 16.38 ± 4.88 (23.85%), 16.67 ± 5.04 (24.29%), and 16.96 ± 5.71 (24.78%), respectively, from baseline to 5, 10, 15, 20, 25, and 30 min. ΔTs values were significantly higher in the successfully blocked patients than in the complete failure patients and contralateral hand at the 30th min. However, there was no statistically significant difference when comparing ΔTs values of successful block and partial failure block patients at the 30th min.
Peripheral nerve blocks are commonly used in regional anesthesia. In recent years, it has become a reliable technique owing to the low complication and high success rates of application using ultrasound (US) [1-3]. However, there are certain difficulties such as Pinaccurate evaluation of block success because available evaluation techniques (cold sensation, pinprick, muscle force, etc.) are composed of subjective tests [4,5]. Additionally, a cooperative patient is an essential requirement, as well as anatomic information and experience, for the successful applicability of these tests [4,5]. A rapid, reliable, and noninvasive assessment method is needed to accurately evaluate block success.
It has been shown that sympathetic blockade which develops due to peripheral nerve block causes vasodilatation and increased peripheral blood flow and consequently leads to elevated distal skin temperature [6-8]. Although elevated skin temperature has been demonstrated, there is no absolute conclusion regarding the advantage of skin temperature in evaluating and predicting the success rate of nerve block.
Near-infrared spectroscopy (NIRS) is a novel, continuous, and non-invasive method for monitoring regional tissue oxygenation of cerebral and somatic beds by providing real-time feedback [9]. NIRS, which was initially used for the assessment of cerebral oxygen saturation, is commonly used nowadays to evaluate somatic tissue perfusion [9].
Assuming that sympathetic blockage can affect tissue oxygen saturation due to vasodilation and increased peripheral blood flow, we hypothesized that the evaluation of tissue oxygen saturation determined by NIRS would be a predictor of peripheral nerve block success.
Institutional ethics committee approval (Necmettin Erbakan University Meram School of Medicine, no. 2016/464) and written consent from the patients were obtained for this prospective, observational study. It has been registered in the Australian New Zealand Clinical Trial Registry (ACTRN12616000656437). Forty patients between the ages of 18-65 years, American Society of Anaesthesiologists physical status I and II, scheduled for acute or elective hand or forearm surgery under lateral infraclavicular block, were studied. Exclusion criteria were age < 18 years, morbid obesity defined as a body mass index (BMI) > 40, international normalized ratio > 1.4, platelet count < 80 × 109 L-1, coagulopathy, medication with vitamin K antagonists, high-dose or fractionated heparin treatment, allergy to local anesthetics, infection at the site of needle insertion, peripheral neurological disease, Raynaud’s phenomenon, and patient refusal. In all patients, a 20-gauge intravenous (IV) cannula was inserted into the radial vein at the wrist of the non-blocked hand for IV fluid and medication administration.
Routine monitoring (consisting of a pulse oximeter, 3-lead electrocardiogram, and non-invasive blood pressure cuff) was performed.
The patients were placed in a supine position in the recovery ward at a room temperature of 21°C. Direct sunlight was avoided, all bandages and clothing were removed from the forearms and hands, and the patients were allowed to acclimatize for 10 min. Both hands remained in a neutral position while the block was performed and during the following 30 min of measurements. A blinded anesthesia nurse recorded skin temperature (Ts) of both hands at baseline, immediately after lateral infraclavicular (LIC) block and at 5 min intervals for 30 min, starting immediately after performing LIC block (LIB). A VeraTempTM V32035 device (Lotus Global Co., UK) was used for skin temperature assessment.
Using a high-frequency linear US transducer (LA435/13−6 MHz, Esaote My Lab Five Mobile Ultrasound System, Esaote, USA), the axillary artery and vein were located in the cross-section of the LIC region and the position of the three nerve cords. After disinfection with ethanol-chlorhexidine (83% and 0.5%, respectively), a sterile transparent drape was placed over the planned injection site, and the attending anesthesiologist performed the LIC block previously described [10] as a triple injection technique, and 10 ml of bupivacaine 0.25% and prilocaine 0.05% was injected into the three nerve cords. We used a lateral and sagittal in-plane US-guided approach to position the needle tip (SonoPlex Stim cannula 22 G 80-100 mm, Pajunk, USA). When correctly positioned, spread of local anesthetics was observed. The blocks were performed by experienced (> 100 performed LIC blocks) and less experienced (between 20 and 100 performed LIC blocks) anesthesiologists.
Immediately after the injection of the local anesthetic, two investigators blinded to the study evaluated the block until the 30th min after the injection. Sensory block was evaluated with sensation to cold elicited by applying ice cubes on the dermatomes of the median (palmar aspect of second finger), radial (dorsum of the hand between thumb and second finger), ulnar (fifth finger), and musculocutaneous (lateral aspect of forearm) nerves, if the patient's hand was eligible for evaluation. The sensation of the patients was recorded as either cold or not cold.
Motor function was assessed by the ability of the patients to extend the wrist (radial nerve), oppose the first digit (median nerve), flex the distal interphalangeal joint of the fifth digit (ulnar nerve), and flex the elbow joint (musculocutaneous nerve). Motor block of each nerve was recorded as either normal or compromised compared with the non-blocked side. Lateral infraclavicular block was categorized as successful when all four nerves were affected by both sensory and motor functions, as described above. In contrast, the block was categorized as failed when any part of the evaluated sensory or motor function remained intact. Patients with successful blocks were transferred directly to the operating room, whereas those with unsuccessful blocks were given a complementary US-guided nerve block (peripheral individual musculocutaneous, ulnar, median, or radial nerve blocks) depending on the failure.
Two sensors (Small Adult SomaSensors, Somanetics, USA) were placed on each patient: one on the side of the peripheral nerve block and another at a similar site on the contralateral side, as described by the manufacturer. The ventral aspect of the mid-forearm area was preferred for sensor placement, as described in a previous study [11]. The sensors were connected to a two-channel monitor (Invos 5100 B monitor, Somanetics) that automatically recorded digital data approximately every 7 s for a maximum of 30 min. A blinded anesthesia nurse recorded bilateral tissue oxygen saturation values from the monitor at baseline, immediately after LIB and at 5 min intervals for 30 min, starting immediately after performing LIB.
Our study was designed to have an 80% power at the 95% significance level to detect an increase in the Ts when the successful block was reached, as reported by Lange et al. [12]. On the basis of this study evaluating Ts (ΔTs = 2.5°C, SD = 3.8), we calculated that 20 patients were required. However, we included 40 patients in the study because the main purpose of the study was to evaluate tissue oxygen saturation with NIRS to predict the success of the LIC block. NIRS values that could have been used in previous studies for sample size calculations could not be determined. Therefore, the sample size was calculated according to skin temperature, which is the secondary outcome of our study.
Statistical analysis was carried out by a statistical software package (SPSS 20.0®, SPSS, USA). Data are expressed as mean ± SD or number of patients. The Wilcoxon signed-rank test was used to analyze changes in mean NIRS values and Ts between baseline and the other measurement times (5, 10, 15, 20, 25, and 30 min) within the blocked and non-blocked hands. To analyze the effects of time (measurement times = 0, 5, 10, 15, 20, 25, and 30 min) and block (successful block, partial failure, complete failure, or contralateral hand) on NIRS values, two-way repeated-measures analysis of variance was used. P values were Bonferroni-corrected. Statistical significance was set at P < 0.05.
Forty patients were enrolled in the study, and all completed the study. Twenty-seven patients underwent elective surgery, and 13 patients were scheduled emergently. No patient withdrew from the study after the LIC block. Thirty-one of the performed LIC blocks were successful, 5 were partial failures, and 4 were complete failures. In a total of 9 failed blocks (complete and partial), the LIC block was successfully repeated preoperatively. Successful block patients did not require additional intraoperative analgesics, and visual analogue scale scores were 0 for 12 h postoperatively. Patient demographic data are summarized in Table 1. There were no significant differences between the three groups regarding sex, age, weight, height, BMI, and American Society of Anaesthesiologists physical status (P=0.436, P=0.459, P=0.906, P=0.774, P=0.826, and P=0.459, respectively).
The NIRS values from the baseline to 30th min are shown in Fig. 1. Baseline NIRS values were 70.84 ± 6.79, 70.20 ± 6.72, 65.75 ± 3.77, and 69.63 ± 8.14 in successful, partial failure, complete failure patients and contralateral side, respectively, and showed no statistical difference (P = 0.834). NIRS values were significantly higher in the successfully blocked patients than in the complete failure patients and contralateral side (P = 0.003 and P < 0.001, respectively) at the 5th min. However, there was no statistically significant difference between NIRS values of successful block patients (81.94 ± 6.82) and partial failure patients (73.80 ± 6.30) at 5 min (P = 0.164). NIRS values were significantly higher in the successfully blocked patients from the complete failure, partial failure, and contralateral sides (P < 0.001, P = 0.008, and P < 0.001, respectively) at the 10th min. There was no statistically significant difference when comparing NIRS values at all measurement times (5th, 10th, 15th, 20th, 25th, 30th min) between complete failure and partial failure block patients (P=0.996, P=0.467, P=0.373, P=0.321, P=0.183, and P=0.261, respectively).
The changes in the Δ NIRS values are shown in Fig. 2. In the successfully blocked patients, NIRS values (mean ± SD [Change in %]) increased by 11.09 ± 4.86 (16.03%), 15.00 ± 4.53 (21.76%), 16.35 ± 5.14 (23.77%), 16.38 ± 4.88 (23.85%), 16.67 ± 5.04 (24.29%) and 16.96 ± 5.71 (24.78%), respectively, from baseline to 5, 10, 15, 20, 25, and 30 min (P < 0.001). Δ NIRS values were significantly higher in the successfully blocked patients than in the partial failure patients, complete failure patients, and contralateral side (P = 0.047, P = 0.002, and P < 0.001, respectively) at the 5th min. Δ NIRS values were significantly higher in the successfully blocked patients from the complete failure, partial failure, and contralateral groups (P < 0.001, P < 0.001, and P = 0.008, respectively) at the 10th min. NIRS values increased by 21.76% in the successfully blocked patients at 10th min according to baseline, whereas this increase was 8.54% in partial failure patients (P = 0.003). NIRS values increased by 24.78%, 10.83%, 1.14%, and -5.26%, respectively, in the successfully blocked, partial failure, complete failure patients and contralateral, from baseline to 30th min (P < 0.001, P = 0.225, P = 0.996, and P = 0.448).
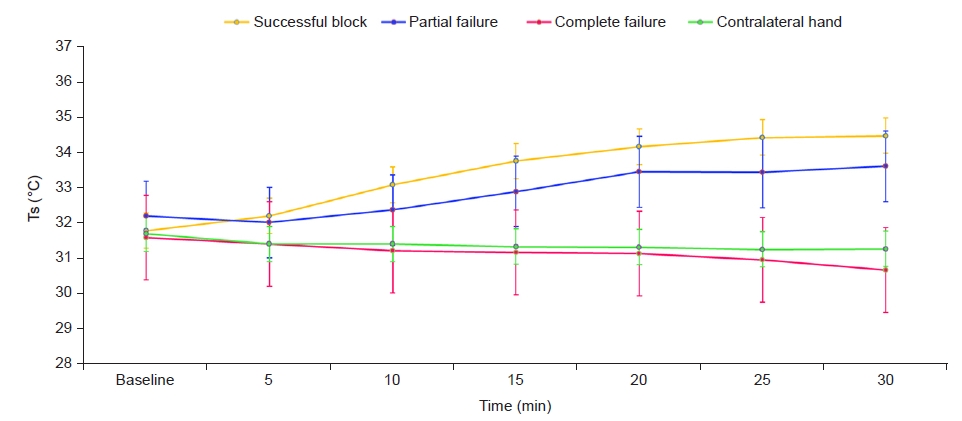
The Ts values from baseline to 30th min are shown in Fig. 3. Ts increased from 31.77 ± 1.28 to 32.19 ± 1.54, 33.07 ± 1.56, 33.74 ± 1.27, 34.15 ± 1.18, 34.41 ± 1.10 and 34.46 ± 1.20 in the successfully block patients from baseline to 5th, 10th, 15th, 20th, 25th, 30th min (P = 0.054, P < 0.001, P < 0.001, P < 0.001, P < 0.001, and P < 0.001, respectively). In the three patients with completely failed blocks, Ts decreased from baseline to 30th min (-0.9°C, -1.5°C, and -0.9°C). However, in one of the patients with complete failure, block Ts increased from baseline to 30th min (0.6°C). In complete failure block patients, skin temperature and Δ skin temperature did not show statistically significant difference from baseline to 30th min (P = 0.366 and P = 0.252, respectively).
Ts in one of the patients with partial failure decreased from baseline to 30th min (-3.9°C). Ts in the remaining four patients with partial failure block Ts increased from baseline to 30th minute (+3.2°C, +2.1°C, +3.6°C, and +1.9°C). In partial failure block patients, skin temperature and Δ skin temperature did not show satitstically significant difference from baseline to 30th min (P = 0.162 and P = 0.156, respectively).
There were no statistically significant differences when comparing Ts values of complete failure and partial failure block patients at all measurement times (5th, 10th, 15th, 20th, 25th, 30th min) (P = 0.992, P = 0.996, P = 0.588, P = 0.185, P = 0.155, and P = 0.063, respectively).
The changes in ΔTs values are shown in Fig. 4. Δ Ts (baseline to 30 min) values were 2.69 ± 1.40, 2.20 ± 1.39, 1.47 ± 2.89, and -0.43 ± 1.11, in the successful block, partial failure, and complete failure patients and contralateral side (P < 0.001, P = 0.223, P = 0.996, and P = 0.102, respectively). Δ Ts values were significantly higher in the successfully blocked patients than in the complete failure patients and contralateral side (P < 0.001 and P = 0.008, respectively) at the 30th min. However, there was no statistically significant difference when comparing Δ Ts values of the successful block and partial failure block patients at the 30th min (P = 0.162).
To the best of our knowledge, this is the first study to evaluate tissue oxygen saturation changes in the forearm and hand according to NIRS responses after US-guided LIC blocks. The essential purpose of this study was to comprehensively evaluate these changes and assess the efficacy of NIRS in predicting blockade success. We planned to define the amount and timing of the changes in NIRS values for evaluation. Beginning from the 10th min after the LIC block, NIRS values in the successful block patients were significantly different compared with partial failure, complete failure patients, and contralateral hand. In the successful block patients, NIRS values showed an increase of 21.76% at the 10th min compared with baseline values, and this increase continued until the 30th min. Completely failed block occurred in only four patients, while partially failed block occurred in five patients. The NIRS values of the successful block patients increased significantly 30 min after the block compared to both baseline NIRS values and those in the partial failure, complete failure patients, and contralateral hand. However, no significant increase occurred in either the NIRS or Ts values of the partial failure patients compared with the complete failure patients.
The other essential purpose of the present study was to define changes in Ts after a successful LIC block. The change in Ts values at 30th min was significantly higher in the successful block patients than in the complete failure patients and the contralateral hand, whereas no significant difference was found compared with partial failure patients.
Local anesthetic agents should be able to block both sensory and sympathetic nerve fibers for a successful block [13]. The clinical control of sensory fibers is evaluated using methods such as cold response and pinprick sensation [13-15]. The blockade of small non-myelinated sympathetic nerve fibers using local anesthetics causes vasodilatation, increased blood flow, and increased local temperature. It is known that sympathetic nerve fibers run peripherally along both major nerves and vessels [16]. In the present study, somatosensors were placed on the ventral aspect of the midforearm. We assumed that this region is the most intensive region for major vascular structures of the forearm and thereby would be the most appropriate site for the evaluation of tissue oxygen saturation.
Changes in Ts and thermography values after upper-extremity peripheral nerve blocks have been evaluated in many studies. Minville et al. [8] evaluated skin temperature after nerve stimulator-guided infraclavicular nerve block. They concluded that the block was successful only if nerve-distribution density increased in four major nerves (musculocutaneous, radial, median, and ulnar nerves). On the other hand, it has been stated in subsequent studies that peripheral blockade of the ulnar and median nerves leads to characteristic increases in hand-skin temperature, whereas peripheral blockade of the radial and musculocutaneous nerves caused no change in hand-skin temperature [12]. The palmar face of the fourth digit which represents a thermographically overlapping area between the median and ulnar nerves, appears to be an ideal area to rapidly and accurately assess the change in distal Ts value [17]. However, the intersection of the median and ulnar nerves makes this area diagnostically insignificant. Therefore, the first, second, and fifth digits are commonly preferred for the evaluation of distal Ts [12,17,18]. On the other hand, in the present study, skin temperature could not be measured at these sites because most of the patients would undergo hand surgery and their digits would be injured and bandaged or casted. Consequently, the skin temperature was measured at the bilateral wrist foldings, which is described in the literature as one of the sites used to evaluate skin temperature after upper extremity peripheral nerve blocks [18].
Asghar et al. [18] have preferred different anatomical regions to evaluate the efficacy of distal infrared thermography and skin temperature in predicting the success of US-guided interscalene brachial plexus in their study. The first, second, and fifth digits were used to evaluate the distal aspect of the hand. The wrist region of the hand was also used in a manner similar to that in our study. They found that skin temperature increased by 3.1°C in the wrists of successful block patients (from baseline to 30th min), whereas our study showed an increase of 2.69°C. Further, it has been noted in this study that the distal Ts of the thumb would be the most appropriate region for the prediction of block success.
Asghar et al. [17] evaluated the change in distal Ts from the second and fifth digits of patients who underwent infraclavicular block in another study and detected a significant elevation at 30th min compared with baseline values in successful block patients. Similar to our results, they stated that no significant change was observed in patients who received the failed block. However, we found no significant difference between patients with successful block and those with partially failed block in terms of the values at the 30th min. We believe that this may be due to the measurement site of Ts used in our study. Additionally, the distal skin temperature is exposed to great fluctuations due to changes in environmental temperature, sympathetic nerve activity (stress, anxiety), local inflammation, and previous trauma. We tried to cool both hands by putting them on cold packages to reduce the effects of these factors and standardize the measurements. However, fluctuations may have occurred because of the procedure itself, as well as the reasons mentioned above.
Thermography studies have become prominent in the successful evaluation of peripheral nerve blocks as well as the measurement of distal skin temperature. It is known that sympathetic nerve fibers run peripherally along both major nerves and vessels [16]. Hence, it may be difficult to predict thermographic patterns at various levels of brachial plexus block, such as axillary brachial plexus block, lateral infraclavicular block, and interscalene brachial plexus block.
Besides the present study, there is still insufficient data on evaluation of the changes in the tissue oxygen saturation based on NIRS responses and efficacy assessment of NIRS in the prediction of block success, whereas the number of studies on distal skin temperature and thermographic assessments to evaluate the success of peripheral nerve blocks have progressively increased. Nerve block was successfully evaluated using NIRS after blockade of the stellate ganglion [19], and it was stated that the use of NIRS would be appropriate to evaluate the success of the nerve block [19,20]. Tighe et al. [11] evaluated tissue oxygen saturation using NIRS after peripheral nerve blocks; however, they demonstrated no significant efficacy. However, these outcomes may be due to the use of a small number of patients, as they have stated, along with the application of various blocks in an identical methodology. In contrast with this outcome, NIRS appears to be an effective method for the prediction of successful block in our study compared with both completely and partially failed blocks beginning from the 10th min following the nerve block procedure. In addition, its practicality and clinical understanding are easier to comprehend than those of thermographic measurements.
In other studies, pulse oximetry and oxygen electrodes following a peripheral nerve block were used to detect changes in tissue oxygenation and perfusion [21-23]. However, none of these methods include non-invasive measurements of the subcutaneous oxygenation state following upper and lower peripheral nerve blocks.
Therefore, we conclude that the assessment of tissue oxygen saturation by NIRS in the evaluation of peripheral nerve block is a rapid, efficient, and practical method. We believe that as the first study in this field, our results would shed light on future studies which will investigate the role of the assessment of tissue oxygen saturation by NIRS in predicting the success of various peripheral nerve blocks.
Notes
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Mehmet Sargın, Mehmet Selçuk Uluer. Data curation: Mehmet Sargın, Mehmet Selçuk Uluer. Formal analysis: Mehmet Sargın, Mehmet Selçuk Uluer. Funding acquisition: Mehmet Sargın. Methodology: Mehmet Sargın. Project administration: Mehmet Sargın. Visualization: Mehmet Sargın. Writing - original draft: Mehmet Sargın. Writing - review & editing: Mehmet Sargın, Mehmet Selçuk Uluer. Investigation: Mehmet Sargın. Resources: Mehmet Sargın. Software: Mehmet Sargın. Supervision: Mehmet Sargın. Validation: Mehmet Sargın.
Fig. 1.
NIRS values from baseline to 30th min of lateral infraclavicular block. NIRS: near-infrared spectroscopy.

Fig. 2.
Changes in Δ NIRS values from baseline to 30th min of lateral infraclavicular block. NIRS: near-infrared spectroscopy.
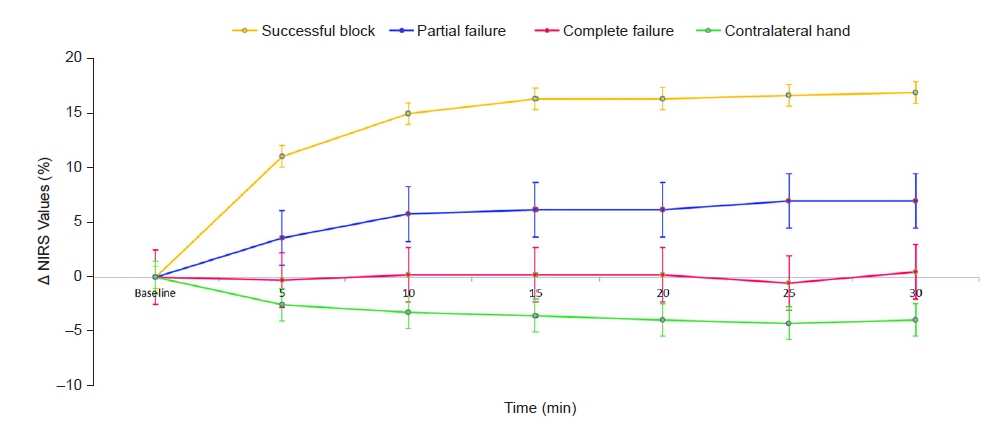
Fig. 4.
Changes in Δ Ts values from baseline to 30th min of lateral infraclavicular block. Ts: skin temperature.

Table 1.
Patient Characteristics
REFERENCES
1. Sandhu NS, Manne JS, Medabalmi PK, Capan LM. Sonographically guided infraclavicular brachial plexus block in adults: a retrospective analysis of 1146 cases. J Ultrasound Med 2006; 25: 1555-61.

2. Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth 2002; 89: 254-9.


3. Arcand G, Williams SR, Chouinard P, Boudreault D, Harris P, Ruel M, et al. Ultrasound-guided infraclavicular versus supraclavicular block. Anesth Analg 2005; 101: 886-90.


4. Curatolo M, Petersen-Felix S, Arendt-Nielsen L. Assessment of regional analgesia in clinical practice and research. Br Med Bull 2005; 71: 61-76.


5. Paqueron X, Gentili ME, Willer JC, Coriat P, Riou B. Time sequence of sensory changes after upper extremity block: swelling sensation is an early and accurate predictor of success. Anesthesiology 2004; 101: 162-8.

6. Galvin EM, Niehof S, Medina HJ, Zijlstra FJ, van Bommel J, Klein J, et al. Thermographic temperature measurement compared with pinprick and cold sensation in predicting the effectiveness of regional blocks. Anesth Analg 2006; 102: 598-604.


7. Hermanns H, Braun S, Werdehausen R, Werner A, Lipfert P, Stevens MF. Skin temperature after interscalene brachial plexus blockade. Reg Anesth Pain Med 2007; 32: 481-7.


8. Minville V, Gendre A, Hirsch J, Silva S, Bourdet B, Barbero C, et al. The efficacy of skin temperature for block assessment after infraclavicular brachial plexus block. Anesth Analg 2009; 108: 1034-6.


9. Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth 2009; 103 Suppl 1: i3-13.


10. Desgagnés MC, Lévesque S, Dion N, Nadeau MJ, Coté D, Brassard J, et al. A comparison of a single or triple injection technique for ultrasound-guided infraclavicular block: a prospective randomized controlled study. Anesth Analg 2009; 109: 668-72.


11. Tighe PJ, Elliott CE, Lucas SD, Boezaart AP. Noninvasive tissue oxygen saturation determined by near-infrared spectroscopy following peripheral nerve block. Acta Anaesthesiol Scand 2011; 55: 1239-46.


12. Lange KH, Jansen T, Asghar S, Kristensen PL, Skjønnemand M, Nørgaard P. Skin temperature measured by infrared thermography after specific ultrasound-guided blocking of the musculocutaneous, radial, ulnar, and median nerves in the upper extremity. Br J Anaesth 2011; 106: 887-95.


13. Yarnitsky D, Ochoa JL. Warm and cold specific somatosensory systems. Psychophysical thresholds, reaction times and peripheral conduction velocities. Brain 1991; 114(Pt 4): 1819-26.

14. Fowler CJ, Sitzoglou K, Ali Z, Halonen P. The conduction velocities of peripheral nerve fibres conveying sensations of warming and cooling. J Neurol Neurosurg Psychiatry 1988; 51: 1164-70.



15. Burke D, Mackenzie RA, Skuse NF, Lethlean AK. Cutaneous afferent activity in median and radial nerve fascicles: a microelectrode study. J Neurol Neurosurg Psychiatry 1975; 38: 855-64.



16. Robertson D, Biaggioni I, Burnstock G, Low PA, Paton JFR. Primer on the autonomic nervous system. 3rd ed. San Diego (CA), Academic Press. 2012.
17. Asghar S, Lange KHW, Lundstrøm LH. Blinded observer evaluation of distal skin temperature for predicting lateral infraclavicular block success. Anesth Analg 2015; 120: 246-51. Erratum in: Anesth Analg 2015; 121: 577.
18. Asghar S, Bjerregaard LS, Lundstrøm LH, Lund J, Jenstrup MT, Lange KH. Distal infrared thermography and skin temperature after ultrasound-guided interscalene brachial plexus block: a prospective observational study. Eur J Anaesthesiol 2014; 31: 626-34.

19. Okano T, Okuda Y, Kimura Y, Mishio M, Shinohara M, Kitajima T. Use of near-infrared spectroscopy to evaluate stellate ganglion block. Reg Anesth Pain Med 2001; 26: 186.


20. Quaresima V, Ferrari M. More on the use of near-infrared spectroscopy to evaluate stellate ganglion block. Reg Anesth Pain Med 2002; 27: 111-2.


21. Galvin EM, Niehof S, Verbrugge SJ, Maissan I, Jahn A, Klein J, et al. Peripheral flow index is a reliable and early indicator of regional block success. Anesth Analg 2006; 103: 239-43.


22. Kabon B, Fleischmann E, Treschan T, Taguchi A, Kapral S, Kurz A. Thoracic epidural anesthesia increases tissue oxygenation during major abdominal surgery. Anesth Analg 2003; 97: 1812-7.


23. Cui W, Kumar C, Chance B. Experimental study of migration depth for the photons measured at sample surface. Proc SPIE 1991; 1431: 180-91.
-
METRICS

-
- 1 Crossref
- 2,446 View
- 62 Download
- Related articles in Anesth Pain Med
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others