Comparison of postoperative back pain between paramedian and midline approach for thoracic epidural anesthesia
Article information
Abstract
Background
The development of back pain following epidural analgesia is one reason for patient refusal of neuraxial analgesia. The primary endpoint of this study was to compare the incidence and severity of back pain following midline and paramedian epidural technique. The secondary endpoint was to identify the risk factors associated with the occurrence of back pain.
Methods
This prospective randomized study included 114 patients receiving thoracic epidural catheterization for pain management following upper abdominal or thoracic surgery. Patients were allocated to either the midline or the paramedian group by computer-generated randomization. An investigator who was blinded to the patient group interviewed patients at 24, and 48 h, and 3–5 days after surgery about the existence of back pain and its severity.
Results
The total incidence of back pain following epidural anesthesia was 23.8% in the midline group and 7.8% in the paramedian group. The numerical rating scale of back pain was not different between the two groups at 24 h and 4 days after surgery. The paramdian technique was associated with a lower incidence of back pain than the midline technique (95% confidence interval 0.05–0.74, odds ratio 0.2, P < 0.01). However, the number of attempts, surgical position, body mass index, and duration of surgery were not associated with back pain.
Conclusions
This study showed that the midline group of thoracic epidural analgesia demonstrated higher incidence of back pain than the paramedian group. However, the pain was mild in intensity and decreased with time in both groups.
INTRODUCTION
One reason for patient refusal of spinal or epidural anesthesia is the fear of back pain following neuraxial anesthesia [1]. Previous study demonstrated that 4% (54/1,191) of patients were not satisfied with spinal anesthesia, and 29% of dissatisfied patients stated that back pain was the reason for their dissatisfaction [1]. The reported incidence of back pain following epidural anesthesia ranges from 2% to 27%. Localized tissue trauma during needle entry and excessive stretching of the supraspinous and interspinous ligaments are possible mechanisms for the development of back pain following neuraxial anesthesia [1,2].
Thoracic epidural analgesia (TEA) is a favored method for the analgesia after upper abdominal and thoracic surgery [3,4]. The thoracic epidural space can be approached via midline and paramedian methods in either the prone or decubitus position [2–4]. In the midline technique, the needle is advanced under the lower margin of the spinous process of the targeted upper vertebrae and passes in the order of the supraspinous ligament, interspinous ligament, ligamentum flavum, and the epidural space. In the paramedian technique, the needle is not advanced between the spinous processes, but is inserted 1 cm lateral and 1 cm caudal to the caudal edge of the spinous process in the sagittal plane. If the paramedian technique is used, the needle encounters the ligamentum flavum without puncturing the supraspinous and interspinous ligaments.
According to a previous study, a large-bore spinal needle during spinal anesthesia resulted in more patients suffering from post-dural puncture back pain due to the increased degree of tissue injury [5]. Suggested risk factors for the development of back pain following epidural anesthesia include preexisting back pain, a higher body mass index (BMI), the size of the Touhy needle, the injection technique, the duration of surgery, the patient’s position during surgery, and the number of needle attempts [1]. Among these risk factors, the effect of the epidural technique on the occurrence of back pain was not specifically investigated. The midline technique always penetrates the spinal ligaments during epidural entry, resulting in the potential occurrence of back pain. Our hypothesis is that not penetrating the supraspinous and interspinous ligaments can reduce the incidence of back pain following epidural analgesia. The primary endpoint of this study is to compare the incidence and severity of back pain following midline and paramedian epidural technique. The secondary endpoint of this study is to identify risk factors associated with the occurrence of back pain.
MATERIALS AND METHODS
Patients
This prospective and randomized study was conducted under the approval of the Institutional Review Board (IRB 2021-03-061). After fully explaining the potential benefits and risks of this study, all patients provided informed consent. This study was registered before patient enrollment at ClinicalTrials.gov (NCT05082220).
Data were collected from March 2021 to November 2021. One hundred and fourteen patients with an American Society of Anesthesiologists physical status classification of I–II, who were aged between 30 and 75 years, were included. The types of surgery included gastrectomy, lung lobectomy, liver lobectomy, and esophagectomy. Patients with preexisting back pain and those who cannot have a conversation or with reduced ability to assess their back pain due to dementia were excluded. Patients with a thoracic spine deformity or congenital anomalies, and a contraindication for epidural analgesia such as allergy to local anesthetics, bleeding tendency and pregnancy were also excluded.
Group allocation
Patients were allocated to either the midline or the paramedian group by computer-generated randomization. All patients in both groups received thoracic epidural catheterization one day before surgery.
Thoracic epidural access
For TEA in this study, all thoracic epidural entries were performed via fluoroscopic guidance in the outpatient pain management clinic one day before surgery. A pain physician with more than 15 years of experience in fluoroscopic guided injections performed all TEAs.
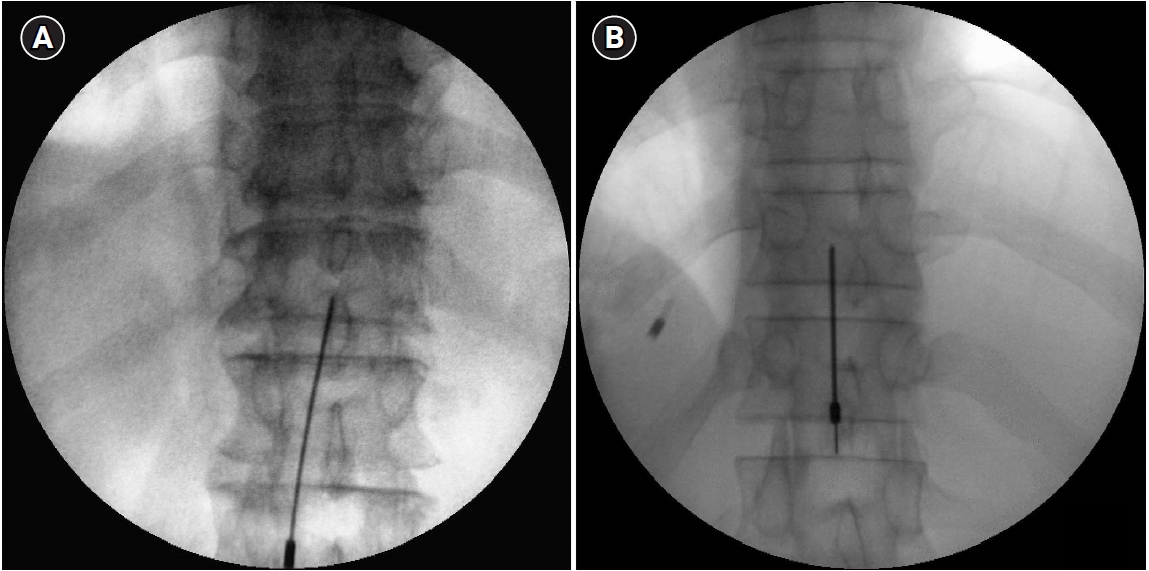
For a paramedian or midline approach of TEA, the interlaminar space of the 9th to the 10th thoracic vertebra was used for epidural entry. In the midline group, the Touhy needle was inserted just below the spinous process of the 9th thoracic vertebra (Fig. 1A). Caudal tilt of 10–15 degree was obtained to enhance the image of interlaminar space. The Touhy needle was advanced slowly until it approached an area near the spinolaminar line in a lateral fluoroscopic view. After determining that the Touhy needle was near the spinolaminar line, the loss of resistance with air was used to confirm the epidural space.
In the paramedian group, the Touhy needle was advanced 1 cm lateral and 1 cm caudal to the caudal edge of the spinous process of the 9th thoracic vertebra (Fig. 1B). Special care was taken that the needle should be inserted away from the midline. It was inserted until it approached an area near the spinolaminar line in a lateral fluoroscopic view. Final confirmation of the thoracic epidural space was determined under fluoroscopic views of anteroposterior and lateral views using 2 ml of contrast medium (Bonorex, 300 mg I/ml).
If the needle was withdrawn completely after encountering the laminae or spinous process with subsequent failure of needle advance, it was considered as first attempt failure.
After the completion of final entry into the targeted epidural space, an epidural catheter was inserted slowly and advanced until the 7th–8th thoracic spine. All patients were equipped with epidural patient-controlled analgesia (PCA) device for 48 h for postoperative pain control. The total volume of epidural PCA was 270 ml, with 300 μg fentanyl (Hana Pharm Co., Korea) and 225 mg ropivacaine (Hanlim Pharm Co., Korea). The epidural PCA was infused at 5 ml/h, and the bolus dose was 5 ml (30 min lock-out times) in all patients.
Patient interview
The patient’s clinical data were recorded, including sex, age, BMI, medical history, method of epidural approach, number of puncture attempts, surgical position, and intravenous rescue analgesics.
The questionnaire to evaluate back pain following epidural analgesia was designed. It did not include transient neurological symptoms such as radicular pain in the buttock, thigh, and calf. An investigator who was blinded to the patient group interviewed patients at 24, 48 h, and 4 days after surgery. At each visit, the same investigator performed the patient interview. An interview one month after surgery was done by telephone. During the interview, we evaluated if the patients had back pain that never experienced before epidural analgesia. If patients showed back pain following epidural analgesia, we asked the severity of pain using a numerical rating scale (NRS). Total incidence of back pain means the sum of patients who showed back pain at 24, 48 h, and 4 days after surgery. The incidence of back at 48 h and 4 days after surgery is a cumulative number of patients.
Patient satisfaction or dissatisfaction was evaluated at the end of this investigation by asking if the patient would choose to receive epidural analgesia again for postoperative pain control.
Statistical analysis
According to the preliminary study, the incidence of low back pain was 10% and 35% in the paramedian and midline groups, respectively. To detect a difference of 0.25 between the two groups, 53 patients in each group were required using a two-sided t-test, with a significance level of 5%, a power of 80%, and a dropout rate of 15%. Continuous variables are presented as mean ± SD or median (interquartile range). Categorical variables are presented as number (percentile). Demographic data and thoracic epidural analgesia with operative data were compared using the chi-square test, unpaired t-test, or Fisher’s exact test. Odds ratios (ORs) were calculated using cross tabulation analysis to identify risk factors associated with the occurrence of back pain (SPSS version 20, IBM Co., USA). A P value of < 0.05 was considered statistically significant.
RESULTS
For possible inclusion in this study, 117 patients were evaluated. Among them, 3 patients refused to participate in this study. Finally, 114 patients completed this study without any dropouts (Fig. 2).
The total incidence of back pain following epidural analgesia was 23.8% (15/63) in the midline group and 7.8% (4/51) in the paramedian group. This incidence of back pain showed a statistically significant difference (P < 0.01). The midline group showed a higher incidence of back pain than the paramedian group and during the time point of 24 (22.3% vs. 6.2%, P < 0.01), 48 h (12.5% vs. 2.3%, P < 0.01), and 4 days (11% vs. 0%, P < 0.01) after surgery. In the time point of 4 days, 12% of the midline group showed back pain, whereas none of the paramedian group showed back pain (Fig. 3). One month after surgery, only 2 patients in the midline group complained of back pain, whereas none of the paramedian group showed back pain.
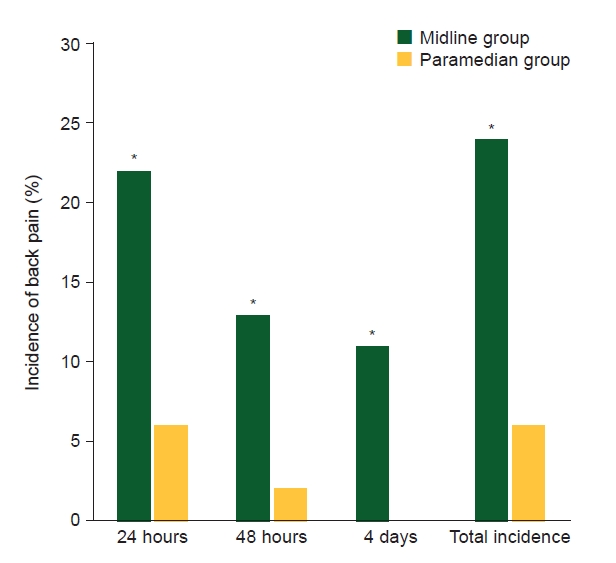
Comparison of incidence of back pain between midline and paramedian groups. The total incidence of back pain following epidural anesthesia was significantly higher in the midline group than the paramedian group. *Statistically significant with P < 0.01.
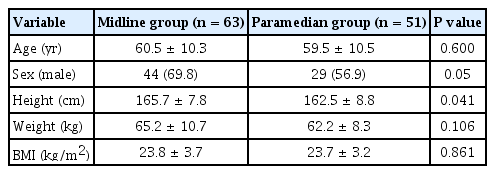
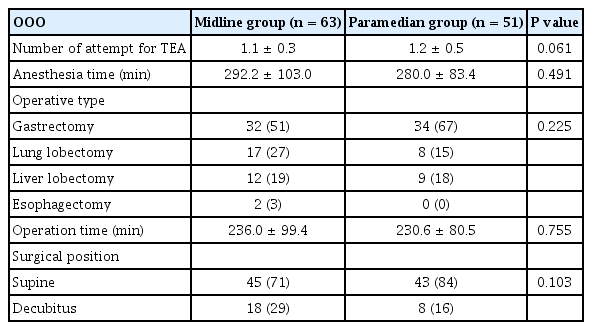
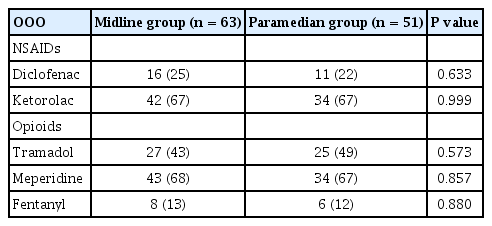
Age and BMI were similar between the two groups. However, in gender distribution, more male patients were included in the midline group than in the paramedian group (Table 1). The number of attempts for TEA, anesthesia and operation times, operative type, and surgical position were similar between the two groups. Among operative types, gastrectomy was most common in both groups (Table 2). In total, 67% of patients in both groups received additional analgesics, including non-steroidal anti-inflammatory drugs and opioids (Table 3). The NRS of back pain was not different between the two groups at 24 h and 4 days after surgery. More than 80% of patients in both groups were satisfied with epidural anesthesia (Table 4). Patients who presented dissatisfaction stated that back pain, inadequate pain control after epidural analgesia, and nausea were reasons for dissatisfaction.
Regarding the association of occurrence of back pain, the paramdian technique was associated with a lower incidence of back pain than the midline technique (95% confidence interval 0.05–0.74, OR 0.2, P < 0.01). However, the number of attempts, surgical position, BMI, and duration of surgery were not associated with the occurrence of back pain (Table 5).
DISCUSSION
The total incidence of back pain following epidural anesthesia was 23.8% and 7.8% in the midline and the paramedian group, respectively in the present study. According to a previous study, the overall incidence of back pain following epidural anesthesia was distributed between 2% and 27% [1]. A higher incidence of back pain in the midline group was observed at 24, 48 h, and 4 days after surgery.
This study excluded patients with preexisting low back pain to prevent any confusion in identifying newly developed back pain following epidural analgesia. Although we did not include patients with preexisting back pain, the risk factors for back pain development after neuraxial anesthesia include preexisting back pain, duration of surgery, lithotomy position, and BMI higher than 32 kg/m2 for proper needle placement [1]. However, this study showed that only the approach method of paramedian technique was associated with a lower incidence of back pain.
Our hypothesis was that the paramedian technique of TEA would demonstrate a lower incidence of back pain because this method does not penetrate the supraspinous and interspinous ligaments. The potential mechanism that initiates back pain following neuraxial anesthesia includes stretching or traumatic injury of ligaments, fascia, or bone with localized bleeding or injury to the adjacent nerve root. Musculoskeletal mechanisms are relaxation of the paraspinal muscles under anesthesia, flattening of the normal lumbar lordosis, immobility of the spine, and stretching of the joint capsules and paraspinal ligaments [1,2,6,7]. Especially, the lithotomy position can cause pelvic rotation, which aggravates the reduction in normal lumbar lordosis [6].
When we perform the midline technique, the large bore needle (17 G) penetrates the midline ligaments, which causes injury or cuttings of supraspinous and interspinous ligaments during needle advancement toward the epidural space. However, the paramedian technique can avoid such injury of midline ligaments by inserting the needle slightly away from the midline. Previous study also showed that spinal anesthesia with the paramedian technique could reduce the incidence of back pain compared to the midline technique [2,8,9]. A recent randomized study demonstrated that the incidence of back pain was 2% and 10% in the paramedian group and the midline group, respectively. However, their study failed in detailed exclusion such as preexisting back pain, immobilization time, and patient position [9].
There are few studies investigating the characteristics or nature of back pain following epidural analgesia. Although this study did not evaluate if the back pain has any radiation to the buttock or lower extremity, most studies report that pain is confined to the back area [1,10,11].
The midline group demonstrated a higher incidence of back pain than the paramedian group, however, the pain was mild in intensity and decreased with time in both groups. One month after surgery, when patients were interviewed about the persistence of back pain, only 3.2% of patients (2/63 patients) in the midline group complained of back pain. A recent study also reported that the incidence of persistent back pain after epidural anesthesia up to 3 months after surgery was only 2% (10/483 patients). Among them, 15% of patients complained of clinically significant back pain 2 days after epidural analgesia, but the pain subsided with time [1,6].
We assessed the level of patient satisfaction of TEA. The midline group demonstrated a higher incidence of back pain, however, patient satisfaction showed a similar distribution between the midline and paramedian groups. Moreover, the level of patient satisfaction was over 80% in both groups. Although back pain developed following epidural analgesia, the intensity was mild, and did not persist for a long time. Therefore, we assume that such a benign nature of back pain affected little on the level of patient satisfaction.
In this study, we compared additional use of analgesics to observe any influence of the approach technique on postoperative pain control. The additional use of analgesics did not show any difference between the two groups, therefore, the approach method did not influence postoperative pain control.
This study includes several limitations. First, the incidence of back pain was evaluated during the immediate postoperative period. Patients in this period were using epidural PCA with intermittent bolus intravenous injection. Therefore, the incidence of back pain in this study could be estimated lower since patients were using epidural and intravenous analgesics during the study period. Second, we focused on identifying the overall incidence of back pain with intensity. Therefore, we cannot suggest the characteristics or nature of back pain. Further study is required to evaluate the characteristics of back pain. Third, a telephone interview, not direct contact, was conducted to evaluate the incidence of back pain 1 month after surgery. Although the evaluation was performed via telephone interview, we think that the existence or absence of back pain was clearly delivered to an interviewer. Fourth, the lithotomy position is known as a possible risk factor of back pain occurrence [1,6]. However, this study did not include the patients with the lithotomy position.
In conclusion, this study showed that the midline group of TEA demonstrated a higher incidence of back pain than the paramedian group. However, the pain was mild in intensity and decreased with time in both groups.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Ji Hee Hong. Data curation: Ji Hee Hong. Methodology: Ji Hee Hong, Ki Beom Park. Writing - original draft: Ji Hee Hong. Writing - review & editing: Ji Hee Hong. Investigation: Ji Hee Hong, Eun Young Cho, Jin Woo Shim, Ki Beom Park.