|
 |
- Search
| Anesth Pain Med > Volume 17(4); 2022 > Article |
|
Abstract
Background
Spinal intramedullary cavernous angioma is a rare form of spinal cord tumor that is associated with myelopathy and significant morbidity and surgical treatment is almost always required.
Case
We report a case of spinal intramedullary cavernous angioma in a pain clinic with initial symptoms of unilateral interdigital space sensory change. MortonŌĆÖs neuroma and piriformis syndrome were clinically suspected, however, symptoms acutely aggravated, and paraplegia developed following the patientŌĆÖs COVID-19 vaccination. Vaccine-associated side effects were ruled out and spinal intramedullary cavernous angioma was confirmed through magnetic resonance image. The patient underwent surgery for complete mass excision.
Conclusions
Recent reports of COVID-19 vaccine-associated side effects have raised sensitive concerns to both health care providers and the public, that in some cases when the symptoms coincide with vaccination history, it may delay time-sensitive diagnosis and treatment and spend unnecessary costs.
Myelopathy is an injury to the spinal cord due to severe compression. Degenerative spinal conditions, like spinal stenosis, spine osteophyte, and disc extrusion, are common causes of myelopathy. Trauma, inflammation, autoimmune disorders, infection, and extradural mass due to metastatic disease are some of the other known causes [1]. A spinal intramedullary cavernous angioma (cavernoma, cavernous malformation) is a rare type of spinal cord tumor that causes a mass effect, acutely progressive myelopathy, hemorrhage, and significant morbidity [2]. We present a case of a patient who presented to our pain clinic with a common symptom of lower limb pain that quickly progressed to myelopathy following administration of the patientŌĆÖs second mRNA SARS-CoV-2 (COVID-19) vaccine.
Institutional Review Board waived the requirement of written consent for the publication of this case (no. BPIRB 2021-11-043).
The patient is a 61-year-old Asian male, with a height of 175 cm and weight of 62 kg, who enjoys walking and is active enough to go hiking almost every day. He was diagnosed with pre-hypertension as his only underlying disease which has been well managed through diet modification and lifestyle changes. A cerebral aneurysm of 2 mm was discovered in a brain magnetic resonance imaging (MRI) with magnetic resonance angiography (MRA) taken for routine medical examination 4 years ago. Since then, a follow-up brain MRA was taken each year and confirmed no changes in aneurysm size.
Pfizer vaccinated the patient for his first mRNA COVID-19 on August 9, 2021, and the next day, he went to a first pain clinic visit due to a sudden onset of paresthesia in the right footŌĆÖs 3rd-4th interdigital space. His initial symptoms were a type of paresthesia, rather than pain. As a result, ultrasonography (USG) was performed with the suspicion of an interdigital neuroma (Morton's neuroma), especially since the patient was a heavy walker and the range of sensory abnormalities was limited to his 3rd-4th interdigital spaces. Except for mild edema around the 3rd-4th interdigital space, no other abnormal findings were present in the USG. It was assumed to be Morton's neuroma due to the typical range of sensory abnormalities, and treatment included educating the patient on the importance of wearing low-pressure shoes, transcutaneous electrical nerve stimulation (TENS), tramadol 25 mg per os (PO) twice daily, and aceclofenac 100 mg PO twice daily.
The patient did not show any improvement of symptoms after one week of treatment, and by the second week, a new pain in his right hip and numbness in the back of his thigh appeared. The pain clinic's anesthesiologist requested a lumbar spine MRI, but no specific findings were found other than mild disc bulging. A thorough physical examination was performed, and the flexion adduction internal rotation test resulted in a positive result. Under suspicion of piriformis syndrome, the patient continued to take the same medication and was prescribed physical therapy such as TENS and hot packs, as well as instruction on proper stretching (Fig. 1). Despite ongoing physical therapy, medication, and stretching, the patient's symptoms did not improve.
The patient went to the emergency room three days after his second mRNA COVID-19 vaccination.
He had fallen asleep and experienced a sudden loss of sensation, paralysis, and electricity-like pain in his entire right leg.
The sensory level of the right foot was less than 60% at the time of admission to the emergency room, and allodynia was noted. Motor power was nearly normal, the deep tendon reflex was intact, and pathological reflexes such as the Babinski and Hoffman reflexes were not seen. The emergency medicine doctor who examined the patient believed that the symptoms began abruptly after the second mRNA vaccination, that no specific findings were found on the previous lumbar spine MRI, and that the symptoms were limited to the right lower extremity. The emergency medicine doctor ordered for low extremity computed tomography (CT)-angiogram, blood fibrinogen degradation production (FDP), and D-dimer laboratory tests to rule out vaccine-related artery thromboembolism. CT-angiogram was normal, and occlusion in the lower extremity blood vessels was not found. The FDP level was less than 2.5, and the D-dimer level was 0.42, which were all within normal range (Fig. 2). Based on these normal results, the emergency medicine doctor concluded that a high possibility exists of peripheral nerve disease that invades the lower extremity nerves and recommended a neurology outpatient department check-up for further evaluation.
The patient's symptoms worsened while waiting for the neurology outpatient appointment date, and three days after returning home from the emergency room, he complained of tingling sensations all over his skin below the navel, significant weakness in his lower extremities, and difficulty passing stool and urine. On physical examination, dorsiflexion and plantarflexion were grade 4, and in the lower extremity, muscle strength and sensations were dull below the T10 dermatome, the deep tendon reflex was normal, and pathological reflexes such as Babinski reflex and Hoffman reflex were not observed. The neurologist suspected acute transverse myelitis, a common side effect of the vaccine, and ordered a whole-spine MRI with gadolinium contrast, an electromyography (EMG), and a cerebrospinal fluid (CSF) study. Steroid pulse therapy (intravenous methylprednisolone 1 g per day) was started while the patient was in the hospital However, after 2 days of steroid pulse therapy, the patient's symptoms worsened rather than improved.
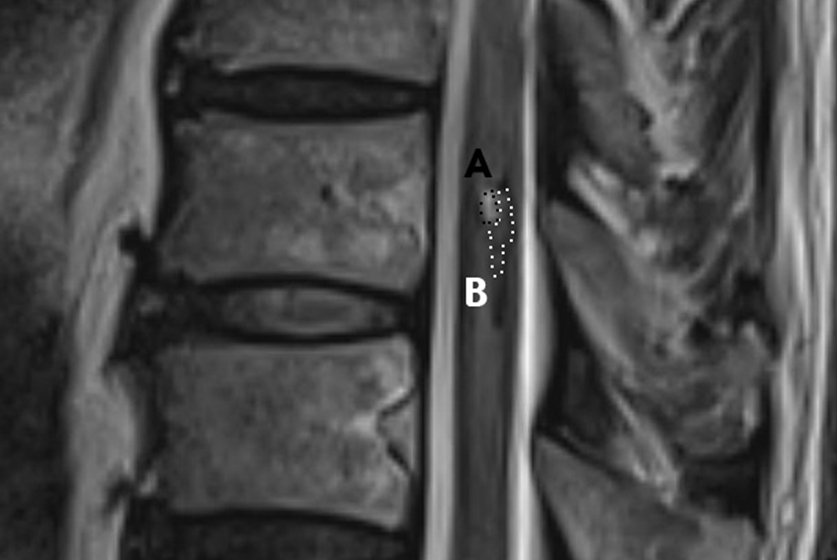
An EMG test performed 2 days later revealed no abnormalities except a decrease in the sensory nerve action potential of the right plantar nerve. Futhermore, neither leukocytes nor erythrocytes were found in the CSF study, making it difficult to believe that there were signs of inflammation. The protein level was also normal as well, indicating concluding that this was not a demyelination disease. The whole-spine MRI with gadolinium contrast revealed findings of a tumor that indicated intramedullary cavernous angioma in the T10 level spinal cord, and hemosiderin deposition was observed around it, indicating signs of previous bleeding. After the MRI image readings were completed, the patient was immediately transferred to another hospital for surgical treatment (Fig. 3).
Surgery involved laminectomy followed by myelotomy, and complete mass excision was performed. Spinal intramedullary cavernous angioma was confirmed through gross and pathological findings during the operation. Two weeks after the operation, the patient still presented with numbness below the T10 dermatome and pain in the right lower extremity, decreased muscle strength in the right lower extremity of motor grade 4 for both dorsiflexion and plantarflexion, and remained stool and urine discomfort. A month after surgery, numbness remained in the dermatome below L2 of right lower extremities, but defecation and urination function had been restored. Additionally, lower extremity muscle strength was restored to 4+, allowing for cane walking. After that, the patient was then transferred to a rehabilitation facility, and further follow-up was impossible.
Cavernous angiomas, also known as cavernomas, are abnormal clusters of small sinusoidal type capillaries and venules that cause a lesion in the central nervous system. Cavernous angioma is most common in the supratentorial cerebral compartment, with prevalence known to be 0.13%. Spinal cavernous angioma is a very rare disease with a prevalence of 0.04-0.05%. Furthermore, most spinal cavernous angioma occurs in the extramedullary region and only rarely in the intramedullary region. The surgical approach for the latter is difficult, and the prognosis is poor [2].
The exact etiology of spinal cavernous angioma has not been elucidated, and incidental detection is rare. Most of the time, the disease progressed far enough that it is discovered much later as a result of symptoms caused by gradually increasing size or neurologic deficits such as pain, radiculopathy, progressive paraparesis, acute paraplegia, and myopathy caused by bleeding and compression. Additionally, if a sudden onset of symptoms occurs, it is often accompanied by hemorrhage, and in this case, early surgical treatment is considered first. Cavernous angioma that is accompanied by sudden onset or rapidly progressive within 1 year exhibits a poor neurological prognosis and can lead to death in severe cases. Therefore, in the case of rapid symptom onset and progression, active surgical treatment is essential as soon as possible [3].
Finsterer and Redzic [4] reported a brainstem cavernous hemangioma hemorrhage that occurred 2 days after the second dose of the mRNA COVID-19 vaccine, the pre-existing vascular malformation might have caused bleeding due to thrombocytopenia or platelet dysfunction after vaccination. Also, Gessler et al. [5] reported 3 cases of intracerebral hemorrhage with thrombocytopenia after vaccination with Oxford/AstraZeneca and Janssen vaccines. In this case, when the patient visited the emergency room after the second vaccination, no thrombocytopenia was found in the complete blood count (platelet count was 240,000 ┬Ąl [normal range: 140,000-440,000 ┬Ąl]). However, by the case report by Radwi and Farsi [6], a systemic subcutaneous hemorrhage was found due to acquired hemophilia that occurred after the COVID-19 vaccination. As a result, we cannot rule out the possibility that the clotting disorder developed and caused hemorrhage for other reasons not affected by the platelet count.
A typical MRI finding of cavernous angioma is hemosiderin deposition by hemorrhage, showing hypointense signals around the lesion [2]. When signals of varying intensities appear in two layers, as in this patient's MRI, it indicates that at least two hemorrhages occurred (Fig. 4). Although the exact bleeding time cannot be estimated based on the information obtained, the bleeding time may be when symptoms worsen rapidly after two doses of the COVID-19 vaccination.
Morton's neuroma is a type of degenerative neuropathy of the interdigital nerve. It is common among middle-aged female, with a lifetime prevalence of 50.2% for men and 87.2% for female [7]. Piriformis syndrome is myofascial referred pain of the piriformis muscle, a pyramid-shaped muscle attached to the upper part of the greater trochanter in the anterior capsule, caused by compression of nerve blood vessels in the great sciatic foramen due to piriformis muscle contraction or thickening. It can cause pain and discomfort during defecation [8]. The patient in this case also showed clinical features of Morton's neuroma or piriformis syndrome, which are mainly seen in pain clinics, manifesting symptoms such as paresthesia between the toes, pain, and paresthesia in the buttocks, and discomfort during defecation. However, no lesions were discovered during radiological examination and physical examinations that are routinely performed at the pain clinic. Furthermore, physical and drug treatment following the presumptive diagnosis was ineffective, and the symptoms worsened rapidly. Given this, even if the symptoms are thought to be of lumbar or sacral nerve origin, considering the possibility of lesions at a higher thoracic or cervical level is important. As a result, comprehensive imaging tests, such as whole-spine MRI, should be considered.
COVID-19 is currently the cause of a widespread pandemic around the world. To prevent transmission between people, new vaccines are being developed at a rapid pace by leading pharmaceutical companies, and vaccination is actively implemented at the national health care level. However, many questions remain about the drug's effectiveness and safety, since it was commercialized in a short period without going through a general clinical trial for a new drug that uses mRNA as a vector for vaccination [9]. A Saudi Arabia study reported that after inoculation with Pfizer's mRNA COVID-19 vaccine, 3.1% of patients presented with lower limb weakness, and 0.3% of patients presented with a loss of lower limb sensation [10]. Other side effects include diseases such as thromboembolism or acute transverse myelitis following mRNA COVID-19 vaccination [11,12]. However, it is too early to conclude that these side effects are related to the COVID-19 vaccine, and no reliable studies exist indicating that these potential vaccination side effects are more dangerous than the disease itself. In this case, the patient was suspected of thromboembolism in the emergency room due to his vaccination history, and a low extremity CT angiogram was taken to rule out vascular occlusion. If the neurologist suspected acute transverse myelitis, he administered steroid pulse therapy. Continuous monitoring of vaccine side effects and appropriate treatment are required. However, concerns about vaccine side effects have been raised by both health care providers and the general public. In some cases, when the symptoms coincide with vaccination history, it may delay time-sensitive diagnosis and proper treatment, furthermore, made unnecessary medical expenses. To summarize, paying attention to vaccine side effects is critical, but it should also be noted that even patients who have a history of COVID-19 vaccination may develop other diseases.
Notes
Fig.┬Ā1.
Lumbar T2 weighted image. Taken when pain in his right hip and numbness in the back of his thigh appeared. There are no specific findings except degenerative changes.

Fig.┬Ā2.
Lower extremity computed tomography angiogram. Taken at emergency room visit with sudden loss of sensation and paralysis in the entire right leg and electricity-like pain. There are no findings suggestive of arterial occlusion, such as thromboembolism.

REFERENCES
1. Oyinkan Marquis B, Capone PM. Chapter 52 - myelopathy. In: Handbook of clinical neurology: neuroimaging part II. Edited by Masdeu JC, Gonz├Īlez RG: Amsterdam, Elsevier. 2016, pp 1015-26.
2. Sun I, Pamir MN. Spinal cavernomas: outcome of surgically treated 10 patients. Front Neurol 2017; 8: 672.



3. Aoyagi N, Kojima K, Kasai H. Review of spinal epidural cavernous hemangioma. Neurol Med Chir (Tokyo) 2003; 43: 471-5; discussion 476.


4. Finsterer J, Redzic Z. Symptomatic peduncular, cavernous bleeding following SARS-CoV-2 vaccination induced immune thrombocytopenia. Brain Hemorrhages 2021; 2: 169-71.



5. Gessler F, Schmitz AK, Dubinski D, Bernstock JD, Lehmann F, Won SY, et al. Neurosurgical considerations regarding decompressive craniectomy for intracerebral hemorrhage after SARS-CoV-2-vaccination in vaccine induced thrombotic thrombocytopenia-VITT. J Clin Med 2021; 10: 2777.



6. Radwi M, Farsi S. A case report of acquired hemophilia following COVID-19 vaccine. J Thromb Haemost 2021; 19: 1515-8.



7. Valisena S, Petri GJ, Ferrero A. Treatment of Morton's neuroma: a systematic review. Foot Ankle Surg 2018; 24: 271-81.


8. Moon DE, Kim YS, Suh JH. The clinical experience of pyriformis syndrome. Korean J Pain 1993; 6: 117-21.
9. Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical students. J Public Health (Oxf) 2021; 43: 445-9.


10. Mohammed RA, Garout RM, Wahid S, Ayub F, Firas ZinAlddin LM, Sultan I. A survey on the side effects of Pfizer/BioNTech COVID-19 vaccine among vaccinated adults in Saudi Arabia. Cureus 2021; 13: e19222.



-
METRICS

-
- 0 Crossref
- 3,654 View
- 58 Download
- Related articles in Anesth Pain Med
-
Liver transplantation of a patient with extreme thrombocytopenia - A case report -2021 July;16(3)
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others