Comparison between GlideRite® rigid stylet and Parker Flex-It™ stylet to facilitate GlideScope intubation in simulated difficult intubation: a randomized controlled study
Article information
Abstract
Background
The GlideScope® videolaryngoscope (GVL) is widely used in patients with difficult airways and provides a good glottic view. However, the acute angle of the blade can make insertion and advancement of an endotracheal tube (ETT) more difficult than direct laryngoscopy, and the use of a stylet is recommended. This randomized controlled trial compared Parker Flex-It™ stylet (PFS) with GlideRite® rigid stylet (GRS) to facilitate intubation with the GVL in simulated difficult intubations.
Methods
Fifty-four patients were randomly allocated to undergo GVL intubation using either GRS (GRS group) or PFS (PFS group). The total intubation time (TIT), 100-mm visual analog scale (VAS) for ease of intubation, success rate at the first attempt, use of laryngeal manipulation, tube advancement rate by assistant, and complications were recorded.
Results
There was no significant difference between the GRS and PFS groups regarding TIT (50.3 ± 12.0 s in the GRS group and 57.8 ± 18.8 s in the PFS group, P = 0.108). However, intubation was more difficult in the PFS group than in the GRS group according to VAS score (P = 0.011). Cases in which the ETT was advanced from the stylet by an assistant, were more frequent in the GRS group than in the PFS group (P = 0.002). The overall incidence of possible complications was not significantly different.
Conclusions
In patients with a simulated difficult airway, there was no difference in TIT using either the PFS or GRS. However, endotracheal intubation with PFS is more difficult to perform than GRS.
INTRODUCTION
The GlideScope® videolaryngoscope (GVL, Verathon, USA) is a novel, commonly used, curved laryngoscope blade with a high-resolution microminiature video camera embedded in the undersurface of the blade, providing a good glottic view. The blade is angled at 60° upwards from the horizontal. The GVL has been widely used and studied to manage patients with difficult airways. However, a stylet is essential for tracheal intubation because of the large angle of the curved blade, which has the potential to make insertion and advancement of an endotracheal tube (ETT) relatively difficult with the possibility of intraoral damage [1].
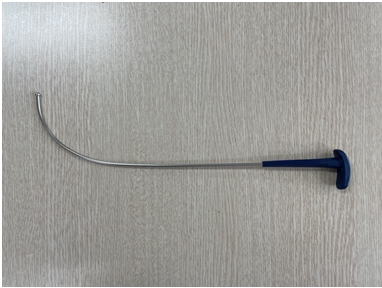
Owing to the curvature of the GVL blade, a stylet must be used to position the ETT tip at the glottic opening [1]. The GlideRite® rigid stylet (GRS) (Fig. 1) is a reusable dedicated stylet provided by the manufacturer with an angle of approximately 90° and radius of 6 cm to fit the GVL [2]. Various authors have recommended different curvatures of the ETT/stylet to optimally place it into the trachea, including matching the blade’s 60° angle, configuring the ETT with a 90° bend [1,3], or using a J-shaped ETT [4]. Other potential strategies may include the use of a flexible stylet that allows active adjustment of the ETT tip angle during tracheal intubation [5]. The Parker Flex-It™ stylet (PFS, Parker Medical, USA) (Fig. 2) is a two-piece plastic stylet allowing active modification of the tip of the ETT during use, and fixation at a specific curvature using a locking clip. Its ability to “relax” the curvature after the ETT tip has passed the vocal cords, facilitates the advancement of the ETT following the curvature of the airway [5,6].

The Parker Flex-It™ stylet (PFS, Parker Medical, USA), shown individually and inserted into an endotracheal tube.
To simulate a difficult airway, we used an adjustable cervical collar, which could be customized for individual cervical lengths. Immobilization using a cervical collar is a method commonly used in patients with cervical spine injuries, and there is no risk caused by the fixation itself [7,8]. This method has been used intentionally to simulate a difficult airway in several previous studies [7,9–11], and different aids for intubation have been studied in simulated difficult airways [7,12]. The Ambu® Perfit ACE cervical collar (Ambu Inc., Denmark) used in this study is different from the rigid or semi-rigid collars used in previous studies [13–15]. It is adjustable to any neck size with 16 different settings ranging from “Neckless” to “Tall” sizes, allowing to size the collar exactly to the individual’s neck size. Therefore, we expected to reconstruct a difficult case precisely.
Previous studies comparing the PFS with the GRS or malleable stylet investigated each stylet in patients with normal airways [5,16]; however, no study has been conducted for difficult airways. Therefore, the purpose of this study was to compare the usefulness of the GRS and PFS during intubation with GVL in a simulated difficult airway, and the alternative hypothesis was that there would be difference in TIT between the two groups.
MATERIALS AND METHODS
This randomized controlled study was approved by the Institutional Review Board of the our hospital (no. 2016-11-005-010). Written informed consent was obtained from all patients before enrollment in the study. The inclusion criteria were patients with American Society of Anesthesia physical status I & II, aged 19–60 years, and scheduled for elective surgery requiring general anesthesia and tracheal intubation. Patients with a body mass index > 35 kg/m2, who needed emergency operations and rapid sequence intubation, had pre-existing dental pathology, and were expected to have difficult airways were excluded from the study. Potentially difficult intubation was defined as the presence of Mallampati class > III, mouth opening < 2.5 cm, thyromental distance < 6 cm, and history of previous difficult intubation.
The patients were randomly assigned to either the GRS group or the PFS group using a random number table generated using the randomization plan generator provided at http://www.randomization.com. In the GRS group, tracheal intubation was performed with the GVL, and the tracheal tube was used with the manufacturer’s stylet, the GRS. In the PFS group, tracheal intubation was performed with PFS.
We recruited 60 patients for this study, and six of them were not eligible because of the Mallampati class IV (n = 2), cancellation of the surgery (n = 2), and invalid informed consent (n = 2) (Fig. 3). The remaining 54 patients fulfilled all criteria and subsequently consented to participate in the study (n = 27 per group). Each patient was allocated to a group using a sealed opaque envelope, which was opened as the patient entered the operating room. The assigned stylet was inserted into the ETT by one of the study investigators, who concealed the stylet and ETT with a towel and then had no further involvement with clinical care or outcome assessment. An independent anesthesiologist, higher than 3rd grade resident doctor who was clinically experienced in handling GVL dozens of times and had practiced intubation with PFS over 30 times to become skilled, performed all tracheal intubations, and was not involved in the collection or analysis of the data.
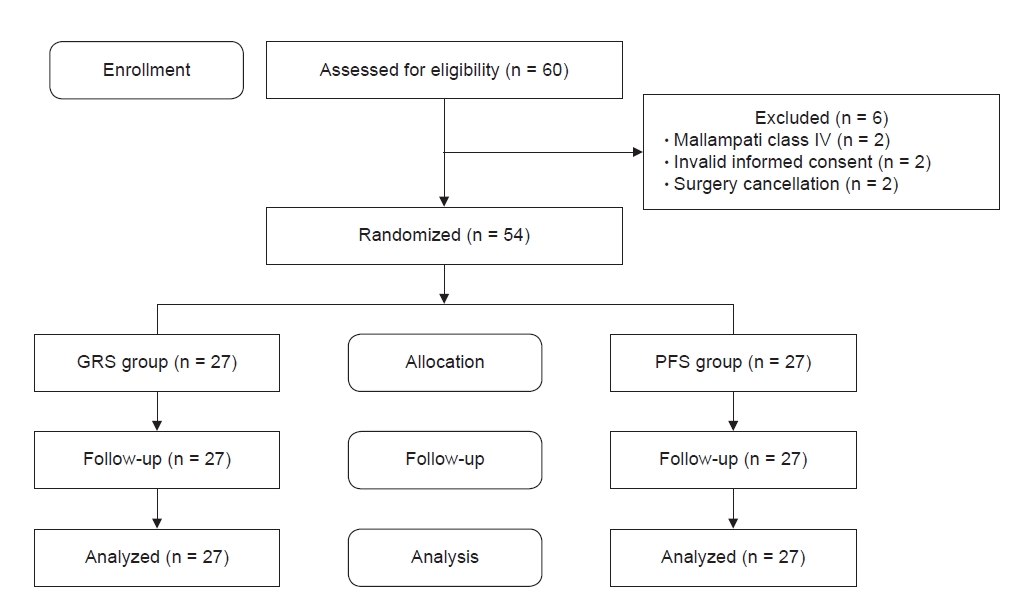
CONSORT flow chart for the study patients. GRS group: GlideRite® rigid stylet (Verathon, USA) group, PFS group: Parker-Flex-It™ stylet (Parker Medical, USA) group.
Before the induction of general anesthesia, we measured the neck circumference, inter-incisor distance (mouth opening), and thyromental distance while awake. After preoxygenation with 100% oxygen for > 3 min, induction was started with 2 mg/kg of 1% propofol and 2 μg/kg of fentanyl. When the patient lost consciousness and manual ventilation with a face mask was well performed, 0.6 mg/kg of rocuronium was administered. Three minutes later, the Cormack-Lehane grade was evaluated using a Macintosh laryngoscope, and the cervical collar was applied to simulate the difficult airway. To evaluate whether the simulated difficult tracheal intubation would be appropriately functioning, the Cormack-Lehane grade was assessed using a Macintosh laryngoscope once more after applying the neck collar. Tracheal intubation was performed using either the GRS or PFS according to each group using 7.5-mm tubes for men and 7.0-mm tubes for women. We allowed the involvement of an assistant with laryngeal manipulation or ETT advancement, if necessary, and recorded it. If the operator removed the GVL blade or ETT from the mouth, this was counted as an additional attempt at intubation.
The primary outcome was total intubation time (TIT), which was defined as the time from insertion of the blade of the GVL into the oral cavity to the appearance of end-tidal carbon dioxide (EtCO2) curve of at least 30 mmHg after intubation of the ETT. TIT was divided into two detailed phases, including endotracheal tube insertion time (EIT) and endotracheal tube advancement time (EAT). After the timer was initiated, the blinded observer measured not only the TIT but also each section of the time. Their definitions are as follows
- EIT: the time from insertion of the blade of the GVL into the oral cavity to the moment just before the ETT contacts the glottic opening.
- EAT: the time from the passing of the ETT through the glottis to the appearance of the EtCO2 curve of at least 30 mmHg on the anesthesia monitor.
Data were collected by one investigator to eliminate observer interpreter bias. We defined failure of tracheal intubation as one of the following cases: three failed attempts, prolonged intubation time > 120 s, or SpO2 < 90% during intubation. In case of failed intubation, we planned to remove the cervical collar and conduct a bag-and-mask ventilation with 100% oxygen, and then perform tracheal intubation with the stylet that the operator preferred to use with the GVL. These cases were excluded from the analysis, and the TIT of the final trial was counted and used for analysis. The time required for intermittent mask ventilation was subtracted from the TIT.
Prespecified secondary outcomes included ease of intubation using a visual analog scale (VAS) (0 = extremely easy to 100 = extremely difficult), the number of attempts, success rate for the first attempt, whether external laryngeal manipulation was used, and whether the ETT was advanced along the stylet by an assistant. During intubation, we also evaluated the occurrence of severe hypoxemia, which was defined as peripheral oxygen saturation (SpO2) < 90%, and laryngospasm. Intraoral examination was performed to confirm the presence of lip, mucosal, or tooth injury immediately after tracheal intubation. After surgery, we examined oropharyngeal trauma with GRS and performed extubation. Subsequently, the presence of blood in the tracheal tube was identified. One hour after the extubation, the patients were interviewed if they had symptoms of complications, such as sore throat, hoarseness, and dysphagia by an independent anesthetist blinded to group allotment in the post-anesthesia care unit; the complications were reevaluated after 24 h in the general ward in the same manner. Hemodynamic data, such as blood pressure, heart rate, and SpO2 were consistently monitored and recorded since the patients entered the operating room until the operation finished, especially before and after tracheal intubation and extubation.
Statistical analyses
The primary outcome was TIT, and the secondary outcomes were VAS score for ease of intubation, success rate at the first attempt, use of laryngeal manipulation, tube advancement rate by assistant, and complications. A pilot study was conducted in 20 patients (10 patients per group) to determine the required sample size. All cases were not included in our present study. The mean ± standard deviation (SD) of the TIT was 52.4 ± 23.1 s for the GRS group and 67.7 ± 14.0 s for the PFS group. Using a statistical significance level of 0.05 (α = 0.05) and 80% power (β = 0.2), we estimated that 26 patients would be required per group. We selected a sample size of 30 patients per group to compensate for potential dropouts (about 10%).
Statistical analysis was performed using the SPSS ver. 23 (IBM Corp., USA). Values are expressed as median (1Q, 3Q), or mean ± SD, or as the number of patients. The normality of the distribution of continuous variables was analyzed using the Shapiro–Wilk test. We used independent t-tests to analyze continuous, normally distributed variables and the Mann–Whitney U test to analyze continuous, non-normally distributed variables. Chi-squared or Fisher’s exact tests were used, as appropriate, for categorical data. The limit of statistical significance was set at P < 0.05.
RESULTS
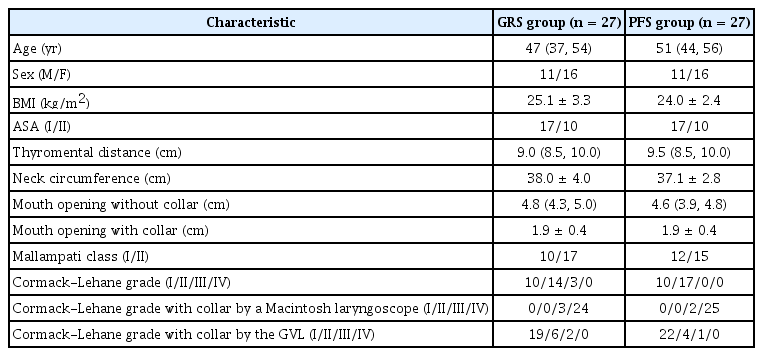
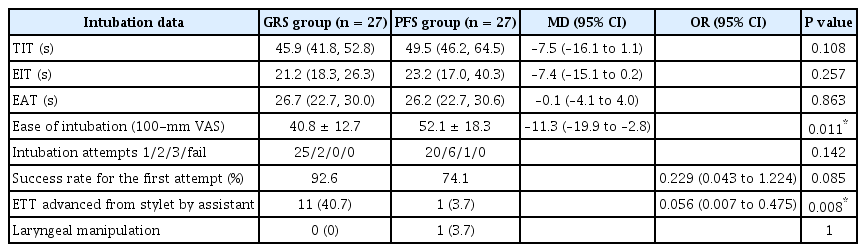
The demographic and airway assessment data of the patients showed no differences between the GRS and PFS groups, as shown in Table 1. All tracheal intubations were successfully performed within three attempts and there were no cases of failed intubation. The Cormack-Lehane grade of the simulated difficult airway evaluated with the Macintosh laryngoscope was greater than III. No statistically significant differences were observed between the two groups concerning the TIT, which was 45.9 s (41.8, 52.8) in the GRS group and 49.5 s (46.2, 64.5) in the PFS group (P = 0.108). The EIT (P = 0.257) and EAT (P = 0.863) also showed no differences between the groups. However, the difference in ease of intubation between the two groups was statistically significant, with a mean VAS score of 40.8 ± 12.7 mm in the GRS group and 52.1 ± 18.3 mm in the PFS group (P = 0.011). The successful tracheal intubation rate at the first attempt was 92.6% in the GRS group and 74.1% in the PFS group (P = 0.142). One case of a third intubation attempt occurred in the PFS group, and the stylets were broken during tracheal intubation in three cases in the PFS group. Cases in which the ETT was advanced along the stylet by an assistant were 11 (40.7%) and 1 (3.7%) in the GRS and PFS groups, respectively (P = 0.002) (Table 2). The incidence of complications, including hypoxemia and dental damage during intubation, was not observed in either group. In addition, there were no significant differences in the incidence of oropharyngeal trauma, blood on the tube, sore throat, hoarseness, and dysphagia between the groups (Table 3). Perioperative hemodynamic data also showed no significant differences.
DISCUSSION
In this study, we assessed the TIT of two different stylets, the GRS and PFS, during tracheal intubation with the GVL in a simulated difficult airway. Our results revealed that there was no difference in TIT using either of the two stylets. We also found that the performance of intubation with the GRS was subjectively easier than that with the PFS according to the VAS score. Less assistance was needed from the assistant in advancing the ETT into the trachea using the PFS in the simulated difficult airway.
The GVL is easy to use and provides a good glottic view during intubation with less cervical movement and lower applied forces; therefore, it is widely used in patients with difficult airways. Despite the excellent glottic visualization provided by the screen of the GVL, it does not guarantee easy and fast tracheal intubation [1]. The dedicated stylet, the GRS, can occasionally make intubation difficult and may impinge on the laryngeal structures around the vocal cords with potential risk of trauma because of its rigidity [17]. Efforts to determine optimal stylets for GVL intubation have been made by many researchers for several years [1,3,4,18]. Although the PFS was originally designed for use with the Macintosh laryngoscope, we expected that the PFS, with its capability to actively angulate the distal ETT, could facilitate insertion and advancement of the ETT during GVL intubation, especially in simulated difficult airways.
Contrary to our expectations, the TIT was not statistically different between the GRS and PFS. We divided the TIT into two phases, namely EIT and EAT. For EIT, we expected that the ETT with the PFS would approach the vocal cords faster than the GRS could because of its flexible feature to actively control the curvature of the ETT following the structure of the airway. For EAT, we expected that the time to advance the ETT/PFS into the trachea would be shortened by releasing the locking clip and relaxation of the active adjustment of the PFS angle, following the natural angle of the ETT, without assistance. However, the EIT and EAT also showed no statistical differences between the two groups. The reason for the absence of differences in the TIT, EIT, and EAT in our study is that handling the PFS is difficult in the limited intraoral space because of the interference of adjacent intraoral structures, unlike in the air without hindrance, thus it could not shorten the EIT. This study showed an advantage regarding the advancement of the ETT off the stylet by an assistant in the PFS group. Only one case (3.7%) in the PFS group needed the help of an assistant while advancing the ETT/stylet into the trachea, while 11 cases (40.7%) in the GRS group required it. It was anticipated that relaxation of the curvature of the PFS after passing the glottic opening would facilitate ETT advancement smoothly, reducing the need for help from an assistant to advance the ETT. However, the PFS group did not present a shorter EAT than that of the GRS group. According to the study by Sheta et al. [16], which investigated the difference in the GRS and PFS in patients with normal airways, PFS had no benefit in shortening the TIT in normal airways.
Tracheal intubation with the GRS was significantly easier than that with the PFS during the use of GVL, based on the VAS score of the experienced operators. However, we need to reconsider the ease of intubation. Careful consideration of the factors that can affect the VAS score is needed. From another perspective, the number of attempts, ability to control the stylet, frequency of usage of external laryngeal manipulation, and advancement of ETT along the stylet by an assistant could influence the evaluation of the VAS score. In our study, even though there were more cases of advancement of ETT requiring an assistant in the GRS group than in the PFS group, difficulty in manipulating the ETT/PFS in the narrow oral cavity, the breakage of the PFS, and a higher frequency of intubation attempts might have resulted in higher VAS scores in the PFS group.
The success rates for the first attempt were 92.6% in the GRS group and 74.1% in the PFS group. Although the difference may not be not statistically significant, but could be clinically significant. It is thought that the rigid GRS was easier to manipulate in the limited intraoral space than the flexible PFS. Repeated intubation attempts in the PFS group were conducted more often than in the GRS group. In three cases in the PFS group, the stylets broke because of their thin and fragile plastic material. In cases of rapid sequence intubation or situations in which successful tracheal intubation must be performed at once, the use of PFS may not be appropriate as a first choice. In such cases, the GRS might be better utilized because of its higher success rate in the first attempt. If the PFS must be used in the first attempt, a “back-up” stylet should be arranged in advance. In addition, we believe that it is necessary to replace the fragile plastic part of the PFS with a durable metallic material.
There is also variation between studies in the type of collar used. In our study, the application of the adjustable cervical collar to the patients facilitated more restricted mouth opening than without the collar, presenting an airway diameter of 4.8 to 1.9 cm in the GRS group and 4.6 to 1.9 cm in the PFS group, thereby sufficiently increasing the Cormack-Lehane grades for glottic view. This implies that the proper simulation of a difficult airway was set up.
Various complications related to the use of the GVL with the GRS or other rigid stylets have been reported by many authors. Previously reported cases of tonsillar and palatopharyngeal injury during intubation with GVL were shown to be related to the rigidity of the stylet and the ‘potential blind spot’ of the GVL [17,19,20]. While concentrating on the GVL monitor to visualize the tip of the ETT adjacent to the glottic opening, a “blind spot” might present in the passage of the styletted ETT from the mouth opening to the vocal cords [17,19]. Our study showed no significant difference in intubation-related complications between the GRS and PFS groups. We first expected that intubation with the PFS would be less traumatic because of its capability to modify the curvature in the oral cavity and its flexible features. Perhaps because of use in the simulated narrow oral environment, both GRS and PFS touched oropharyngeal and laryngeal structures with higher frequency than in the normal airway. The incidence of sore throat 1 h after surgery has been reported as 18.3% in the normal airway [16] and was 50.0% in this study, irrespective of the type of stylet. Moreover, the incidence of oropharyngeal trauma has been reported as 10.0% in the normal airway [16] and was 22.2% in this study. Although the studies were not compared under the same design, the incidence of trauma was higher when intubation was performed in a narrow oral cavity in a simulated difficult airway.
This study has several limitations. First, since most anesthesiologists including the operator in this study are usually familiar with use of the GRS, there might be a possibility of difference in learning curve from that of the PFS. In order to overcome this point, the operator had sufficiently practiced intubation using the PFS prior to study participation. However, we think that it is inevitable that the differences in the learning curve of using the GRS and PFS can sometimes occur, which might have affected estimation of the sample size. If the sample size increases, it could make a statistically significant difference, but it will not be a clinically significant difference. Therefore, the authors believe that the conclusions will be the same as this study. This is one of the major study limitations. Second, the anesthesiologist who performed tracheal intubation could not be blinded to the stylet used. Although the assigned stylet and ETT were concealed before intubation, it was impossible to prevent the anesthesiologist from knowing which stylet was being used during intubation. Third, we tried to simulate a difficult airway with a cervical collar, but it could not reflect an actual difficult airway. Difficult airways include not only neck immobilization and limited mouth opening, but also many structural problems of the airway. Tongue swelling, abnormal dentition, and distorted pharyngeal or laryngeal anatomy can affect the difficulty of tracheal intubation. Therefore, this simulated method is limited in reflecting the actual difficult cases.
In conclusion, in patients with a simulated difficult airway, there was no difference in TIT using either the PFS or GRS. However, endotracheal intubation with the PFS is more difficult to perform than with the GRS.
Acknowledgements
Flex-It™ stylet has been changed manufacturer name since submitting a manuscript (changed from Parker Medical to Salter Labs).
Notes
FUNDING
This study was supported by 2017 Kangwon National University Hospital Grant.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Minsoo Kim. Data curation: Juyoun Kim, Byeongmun Hwang, Songsik Kang. Writing - original draft: Ji Won Bak, Yeonji Noh. Writing - review & editing: Minsoo Kim. Supervision: Heejeong Son.