|
 |
- Search
| Anesth Pain Med > Volume 16(3); 2021 > Article |
|
Abstract
Background
Methods
Results
Notes
DATA AVAILABILITY STATEMENT
The datasets generated durig and/or analyzed during the current study are available from the corresponding author on resonable requet.
AUTHOR CONTRIBUTIONS
Data curation: Ji Hee Hong. Formal analysis: Ji Hee Hong, Ji Hoon Park. Funding acquisition: Ji Hee Hong. Methodology: Ji Hee Hong. Project administration: Ji Hee Hong. Writing - original draft: Ji Hee Hong. Writing - review & editing: Ji Hee Hong. Investigation: Ji Hee Hong, Ji Seob Kim, Hyung Jun Kim. Resources: Ji Hoon Park. Supervision: Ji Hee Hong.
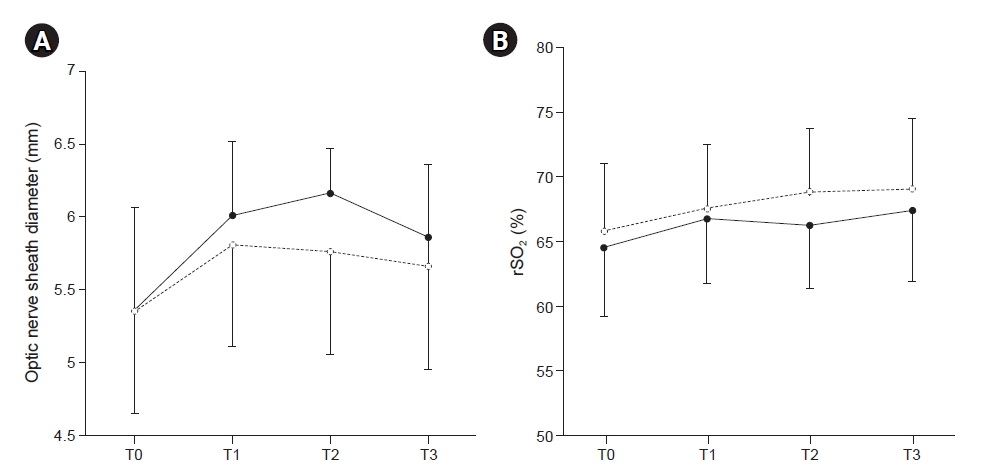
Fig.┬Ā1.
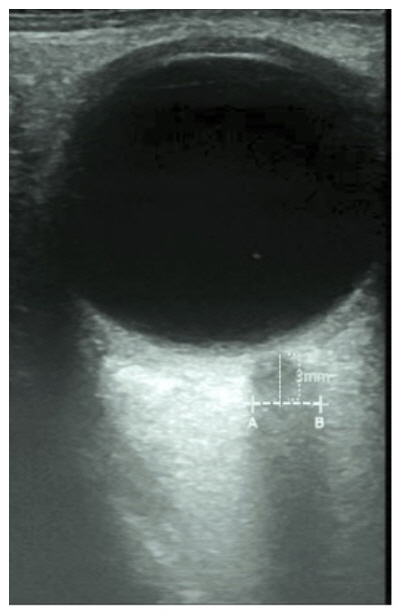
Fig.┬Ā2.
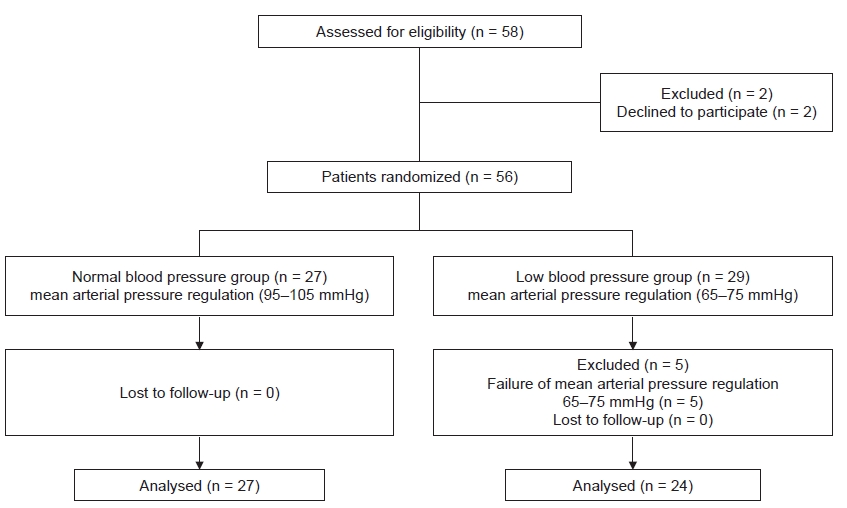
Fig.┬Ā3.
Table┬Ā1.
Table┬Ā2.
Values are presented as mean ┬▒ SD. Adjusted P value indicates the Bonferroni-corrected P value. T0, supine position before anesthesia induction (baseline); T1, 1 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T2, 2 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T3, 10 min after returning to supine position without CO2 pneumoperitoneum at the end of surgery.
Table┬Ā3.
Values are presented as mean ┬▒ SD. Adjusted P value indicates the Bonferroni-corrected P value. T0, supine position before anesthesia induction (baseline); T1, 1 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T2, 2 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T3, 10 min after returning to supine position without CO2 pneumoperitoneum at the end of surgery.
Table┬Ā4.
| Optic nerve sheath diameter and changes in diameter | Normal blood pressure group (n = 27) | Low blood pressure group (n = 24) | Adjusted P value |
|---|---|---|---|
| Optic nerve sheath diameter (mm) | |||
| ŌĆāT0 | 5.31 ┬▒ 0.48 | 5.33 ┬▒ 0.46 | 0.891 |
| ŌĆāT1 | 6.0 ┬▒ 0.47* | 5.82 ┬▒ 0.5ŌĆĀ | 0.631 |
| ŌĆāT2 | 6.1 ┬▒ 0.59ŌĆĪ | 5.77 ┬▒ 0.47ŌĆĀ | 0.121 |
| ŌĆāT3 | 5.87 ┬▒ 0.45 | 5.71 ┬▒ 0.57 | 0.772 |
| Changes in optic nerve sheath diameter (mm) | |||
| ŌĆāT1-T0 | 0.69 ┬▒ 0.37 | 0.49 ┬▒ 0.50 | 0.213 |
| ŌĆāT2-T0 | 0.79 ┬▒ 0.50 | 0.44 ┬▒ 0.50 | 0.142 |
| ŌĆāT3-T0 | 0.56 ┬▒ 0.43 | 0.38 ┬▒ 0.61 | 0.681 |
Values are presented as mean ┬▒ SD. Adjusted P value indicates the Bonferroni-corrected P value. T0, supine position before anesthesia induction (baseline); T1, 1 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T2, 2 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T3, 10 min after returning to supine position without CO2 pneumoperitoneum at the end of surgery.
Table┬Ā5.
Values are presented as mean ┬▒ SD. Adjusted P value indicates the Bonferroni-corrected P value. T0, supine position before anesthesia induction (baseline); T1, 1 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T2, 2 h after 30-degree Trendelenburg position with CO2 pneumoperitoneum; T3, 10 min after returning to supine position without CO2 pneumoperitoneum at the end of surgery.
REFERENCES
-
METRICS

-
- 2 Crossref
- 4,757 View
- 95 Download
- Related articles in Anesth Pain Med
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others