Does the minimal occlusive volume technique provide adequate endotracheal tube cuff pressure to prevent air leakage?: a prospective, randomized, crossover clinical study
Article information
Abstract
Background
Methods of determining proper endotracheal tube (ETT) cuff pressure to prevent air leakage include the minimal occlusive volume (MOV) technique, which uses auscultation, and the spirometer technique, which directly measures inspiratory and expiratory breathing volumes. Spirometers may measure even small air leakage, therefore, the spirometer technique requires a higher cuff pressure than the MOV technique to completely seal the airway. This study aimed to evaluate the difference in cuff pressure between the two techniques used to seal the airway.
Methods
Thirty-five female patients were intubated using an ETT with a cuff, and cuff inflation was performed with both techniques at a 10-min interval in random order—the MOV technique and then the spirometer technique or vice versa. The cuff pressure was measured at each period.
Results
The cuff pressures were 16.7 ± 4.4 cmH2O and 18.7 ± 5.2 cmH2O for the MOV and spirometer techniques, respectively. The cuff pressure for the spirometer technique was 2.0 cmH2O higher than that for the MOV technique and this difference was statistically significant (95% confidence interval, 0.7–3.3; P = 0.003). Considering the upper end (3.3 cmH2O) of the 95% confidence interval and the size of one scale unit (2.0 cmH2O) of a manometer, the difference in cuff pressure was up to 4 cmH2O in practice.
Conclusions
Even though the air leakage sound disappears on auscultation, unlike the previous recommendation, the airway sealing would be completed only by increasing the cuff pressure by approximately 4 cmH2O.
INTRODUCTION
The endotracheal tube (ETT) with a cuff is generally used in mechanically ventilated patients. ETT cuff sealing is necessary to ensure mechanical ventilation with adequate tidal volume and to prevent aspiration [1,2]. A higher cuff pressure can result in complete airway sealing without air leakage, however, increased cuff pressure can contribute to tracheal injuries [3–7]. Therefore, it is important to maintain proper cuff pressure that guarantees airway sealing without overinflating the ETT cuff.
Among various cuff inflation methods to seal the airway, are the minimal occlusive volume (MOV) technique using auscultation and the spirometer technique that directly measures inspiratory and expiratory breathing volumes. The MOV technique has the advantage that it can be easily applied with a stethoscope after tracheal intubation [8–10], while the spirometer, which is embedded in an anesthesia station, has the advantage of being able to monitor the air leakage in real time, and to be a more accurate method to confirm the existence and the degree of the air leakage [10].
Previous studies have reported higher cuff pressures for the MOV technique [10–12] than for the spirometer technique. However, we expected that the cuff pressure determined by the spirometer technique would be higher than that determined by the MOV technique because a spirometer is able to detect even small air leakage. A difference in cuff pressure beyond the minimum measurement unit (2 cmH2O) of the manometer between the two techniques cannot be neglected; therefore, the cuff pressure should be adjusted for the complete sealing of the airway. Hence, this study aimed to compare the cuff pressure using the two techniques with a mean difference of 2 cmH2O.
MATERIALS AND METHODS
This prospective randomized crossover clinical study was approved by the Institutional Review Board of the Dongguk University Ilsan Hospital (no. DUIH IRB 2017-10-004) and was registered on www.clinicaltrials.gov (no. NCT03385044). Written informed consent was obtained from the patients who met the eligibility criteria. Thirty-five patients aged between 20 to 60 years who were scheduled for elective laparoscopic gynecologic surgical procedure from March to October 2018 were included. Each patient was intubated and cuff inflation was performed with both techniques at a 10-min interval in random order—the MOV technique first and then spirometer technique (a spirometer built in an anesthesia machine [Carestation 650™, Datex–Ohmeda Inc., USA], Sequence MS) or vice versa (Sequence SM). The cuff inflation and pressure were measured only once in each technique. Patients with an anticipated difficult intubation, having a history of difficult intubation, body mass index > 30 kg/m2, and known anatomical laryngotracheal abnormalities were excluded.
General anesthesia was induced using an intravenous bolus of propofol 2 mg/kg, remifentanil infusion of 2.0 ng/ml using target-controlled infusion, and the neuromuscular blockade was achieved with rocuronium 0.6 mg/kg. After confirming that the patients were been fully relaxed, they were intubated with a 7.0 mm internal diameter endotracheal tube (TaperGuard™ Oral/Nasal tracheal Tube, Covidien, Mexico). After the endotracheal intubation was performed, we inflated the cuff balloon with air, using a 10-ml syringe until the cuff pressure reached 30 cmH2O. The cuff was progressively inflated by injecting air in 0.5 ml increments until it reaches 30 cmH2O. The measurement was taken with a manometer (VBM Medizintechnik, Sulz am Neckar, Germany) connected to the cuff balloon with a three-way stopcock. The cuff pressure was measured at the end of expiration. Anesthesia was maintained with sevoflurane 1.5–2.0% in combination with air and oxygen at the fraction of inspired oxygen of 0.4. The patients were ventilated using a volume-controlled ventilation with 2.0 L/min of fresh gas flow. After the patient was positioned and carbon dioxide insufflation for the laparoscopic surgery was performed, the tidal volume and the respiratory rate were set to reach a peak inspiratory pressure of 25 cmH2O, which was maintained till the end of the study. Subsequently, the initial ratio of expiration to inspiration volume (VE/VI ratio) was measured. The manometer was connected to a 10-ml syringe and the pilot balloon of the endotracheal tube via a three-way stopcock. After stabilization for 5 min, the cuff was completely deflated. The cuff was considered empty when no more air could be removed on aspiration with the syringe.
The 35 patients were randomly allocated via opaque sealed envelopes to either Sequence MS or Sequence SM (Fig. 1) using internet-based random numbers (http://www.randomizer.org). The random number generation and allocation process was managed by a researcher who did not perform the techniques and data collection. While the patients and data analyst were blinded to allocation, the researcher, who performed the two techniques during the study period could not be blinded to the allocation.

Study protocol. Patients in Sequence MS received the minimal occlusive volume technique during the first period and the spirometer technique during the second period. Patients in Sequence SM were treated in the reverse order. MOV: minimal occlusive volume.
Patients in Sequence MS received the MOV technique during the first period and the spirometer technique during the second period. Patients in Sequence SM were treated in the reverse order. There was a 10 min interval with a cuff pressure of 30 cmH2O between the two periods. The cuff pressure and the volume of air injected into the cuff were measured and recorded by an anesthetic nurse who did not participate in this study. The cuff pressure was measured at the end of expiration when the airway pressure is the lowest in a respiratory cycle. In the MOV technique, after checking that the cuff had been completely deflated, the cuff was then slowly inflated with 0.2 ml increments at every inspiratory moment until the air leakage sound disappeared. The air leakage sound was identified with a stethoscope at the mouth of the patient to ensure the absence of the air leakage. When the air leakage sound disappeared, the cuff pressure and the volume of air injected into the cuff were recorded. In the spirometer technique, after the cuff was completely deflated, the cuff was slowly inflated with 0.2 ml increments using a syringe. The cuff was inflated in each patient during the inspiratory phase. When the final VE/VI ratio of the spirometer reached the initial value, the cuff pressure and the volume of air injected into the cuff were recorded.
After all the measurements in each patient, the cuff pressure was maintained at a value for which no leakage existed throughout the rest of the surgery.
Statistical analysis
The primary outcome was the cuff pressure at the moment when the air leakage disappeared, which was confirmed by the two techniques. The secondary outcome was the volume of air in the cuff when the air leakage disappeared. Clinical studies that have studied clinical complications due to cuff pressure, generally set a difference above 5 cmH2O as a significant difference [13]. However, since this study is looking at the difference in cuff pressure associated with air leakage prevention, we set 2 cmH2O to be the minimum unit of measurement and measurement error, to determine a difference in the cuff pressure. In other words, if it is more than this difference, cuff inflation should be adjusted for adequate sealing.
According to the prior study [14], it is established that the standard deviation of pressure of the ETT cuff that was sealed using MOV technique is 3.8 cmH2O. Given the expected pressure difference of 2 cmH2O, 31 patients were required for a significance level of 0.05 and power of 80% applying a crossover design. Thirty-five patients were recruited considering the dropout rate of 10%.
Data were check for normality with QQ plots. The cuff pressure and the air volume were analyzed using linear mixed models that included the two sealing techniques, sequence MS/SM, and periods, with a random effect for each patient [15]. The initial VE/VI ratio and the final VE/VI ratio were compared using paired t-tests.
R software version 3.5.2 (R Core Team, 2018; https://www.r-project.org/) and additional nlme library (R package version 3.1-137, Pinheiro J, Bates D, DebRoy S, Sarkar D and R Core Team, 2018; http://CRAN.R-project.org/package=nlme) were used for data entry and analysis. Data were presented as mean ± standard deviation or mean difference (95% confidence interval [CI]). Statistical significance was defined as P < 0.05.
RESULTS
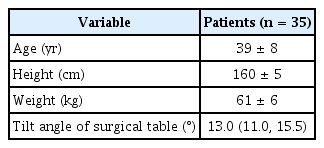
Table 1 shows the demographic characteristics of the patients enrolled in the study. There were no carryover and period effects on cuff pressure and cuff volume. The cuff pressure was 16.7 ± 4.4 cmH2O in the MOV technique, while a cuff pressure of 18.7 ± 5.2 cmH2O was measured in the spirometer technique. The cuff pressure difference between the two sealing techniques was 2.0 cmH2O (95% CI, 0.7–3.3; P = 0.003), which means that the cuff pressure by the spirometer technique was approximately 3.3 cmH2O higher than those of the MOV technique (Table 2).
The difference between the volume of the air in the cuffs was 0.3 ml (95% CI, 0.1–0.5; P = 0.013), which means that the volume of the air in the cuffs sealed by the spirometer technique was approximately 0.5 ml larger than those sealed by the MOV technique (Table 2).
In the spirometer technique, the initial VE/VI ratio measured at the beginning of the study were compared with the final VE/VI ratio at the time when there was no air leakage. No significant difference was observed between the initial VE/VI ratio and the final VE/VI ratio (0.976 ± 0.021, 0.975 ± 0.020, respectively, mean difference = 0.001, 95% CI, –0.002 - 0.004; P = 0.539).
DISCUSSION
As expected, the cuff pressure in the spirometer technique was higher than the cuff pressure in the MOV technique, which was as high as 2.0 cmH2O (95% CI, 0.7–3.3). In other words, even though the sealing was determined by auscultation, a higher cuff pressure was required to seal the airway completely. Considering the 95% CI, the difference is up to 3.3 cmH2O, which also exceeds the manometer's margin of error. Therefore, after the air leakage sound disappears during the MOV technique, the cuff pressure should be increased by two scale units (approximately 4 cmH2O) of a manometer to prevent air leakage. This cuff pressure difference is less than 5 cmH2O, which is meaningful in clinical studies of airway complications associated with high cuff pressure [13]. Furthermore, the increased cuff pressure would not reach the recommended cuff pressure of 30 cmH2O from the guidelines [16,17]. Hence, increasing the cuff pressure about 4 cmH2O would not add to the risk of clinical complications. If the cuff pressure cannot be measured, consider adding 0.5 ml air which is the upper limit of the 95% CI.
Unlike previous studies [10–12], this study showed that the cuff pressure was low when measured by the MOV technique. We slowly inflated the cuff with air with 0.2 ml increment at every inspiratory moment until the air leakage sound heard by the stethoscope disappeared. This precise and stepwise inflation of the cuff may have resulted in the lower cuff pressure without air leakage sounds from the MOV technique.
Many anesthesiologists check the appropriateness of the sealing by referring to the cuff pressure through manually palpating the ETT pilot balloon. They stop inflating the pilot balloon when they feel it is tight enough. However, digital balloon palpation corresponds poorly with the measured ETT cuff pressure [18–20]. Furthermore, when the anesthesiologists manually palpate the pilot balloon to measure the pressure, they usually underestimate them causing over-inflation of the cuffs [8,9]. Hence, it is important to seal the airway using proper methods for the patients’ safety. Humans’ sensitivity for hearing sound is different individually. In other words, one can hear a leakage sound to some extent, while the other one cannot hear the fine or detail sounds caused by the air leakage. The operating room noise will also interfere significantly. For these reasons, some researchers regard that the MOV technique could result in an inadequate airway sealing, with either very high or very low cuff pressures [21,22].
Using the spirometer technique which we have dealt with, physicians now can continuously monitor the air leakage. It can be achieved using a spirometer already built in the anesthesia machine by checking inspiratory and expiratory volumes just like the spirometer technique performed in this study. Sealing ETT cuff properly and monitoring the air leakage continuously would contribute to patients’ safety.
Cuff pressure difference of 2.0 cmH2O (95% CI, 0.7–3.3) may look insignificant, and may be regarded as a measurement error or as the minimum measurement unit of the manometer that can be ignored. However, in this study, we found out the fact that a small amount of the air leakage still exists when the ETT cuff is sealed using the MOV technique. This indicates that when using the MOV technique, an additional pressure of approximately 4 cmH2O is required to completely seal the airway without leaking air.
This study has some limitations. This study included only female patients undergoing gynecological surgery. Therefore, the study results may not be applicable for males or other sizes of ETT, but we tried to reduce other variables by using the same ETT (7.0 mm) size in patients with similar characteristics. In addition, it would be helpful if there was VE/VI ratio at the time the air leakage sound disappeared in the MOV technique. However, since many studies on air leakage used cuff pressure, this study also determined the presence of air leakage based on cuff pressure. Therefore, it was expected that even if the VE/VI ratios were measured directly in the MOV technique, it would not be significantly different from the results of this study. Nevertheless, further research on direct measurement would be helpful.
In conclusion, even if the air leakage sound disappears on a stethoscope in the MOV technique, air leakage may still occur. Therefore, unlike the previous recommendation, the airway sealing would be completed only by increasing the cuff pressure by approximately 4 cmH2O. Further, if the cuff pressure cannot be measured, adding 0.5 ml of air into the cuff would be helpful.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization: Junyong In, Ha Yeon Park. Data acquisition: Mina Kim. Formal analysis: Junyong In. Supervision: Junyong In. Writing—original draft: Ha Yeon Park, Mina Kim. Writing—review & editing: Ha Yeon Park, Junyong In.