Anesthetic management with extracorporeal membrane oxygenation in a patient with acute airway obstruction after inhalation burn injury -A case report-
Article information
Abstract
A 36-year-old woman was admitted to the intensive care unit because of an inhalation burn injury. Five days after admission, she developed dyspnea and hypercarbia. Therefore, fiberoptic bronchoscopy was performed through the endotracheal tube, which revealed foreign bodies in the tube. Tracheostomy was performed to remove, albeit incompletely, the foreign bodies (endotracheal debris). As sudden movement of the patient or airway reaction could cause the foreign bodies to move deeper into the bronchus during manipulation of the rigid bronchoscope, general anesthesia was induced and maintained by using total intravenous anesthesia with extracorporeal membrane oxygenation (ECMO). The foreign bodies were successfully removed without any other complications. This case showed that sloughed endobronchial debris after an inhalation burn injury caused acute airway obstruction. In such cases, alternative ventilation methods such as tracheostomy and ECMO may have to be applied, which can support a surgeon to focus on the procedure regardless of prolonged procedural time.
INTRODUCTION
Inhalation injury is generally defined as a direct thermal injury of the upper or lower airway by the aspiration of superheated gases or chemical injury of the airway caused by the inhalation of noxious gases [1]. Inhalation burn injury has a risk of causing various airway complications such as upper airway obstruction due to secondary edema, reactive bronchospasm from aerosolized irritants, and lower airway obstruction by sloughed endobronchial debris. Lower airway thermal injury caused by the aspiration of products of incomplete combustion can cause sloughing of the airway epithelium, which can lead to the development of complete upper airway obstruction [2]. Several case reports have documented airway obstruction from inhalation burn injuries; nevertheless, few reports have documented abrupt lower airway obstruction caused by endobronchial debris. We encountered an interesting case of lower airway obstruction caused by sloughed endobronchial tissue debris in a patient with inhalation burn injuries. Here, we describe the successful perioperative anesthetic management of a patient with near-complete airway obstruction and establish the usefulness of extracorporeal membrane oxygenation (ECMO) support during bronchoscopy to resolve the airway obstruction.
CASE REPORT
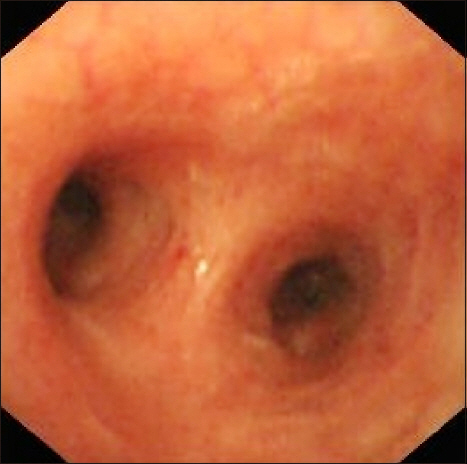
A 36-year-old woman was admitted to the emergency department with a suspicion of inhalation burn injury due to a fire at her home. She was drowsy at presentation. Initial arterial blood gas analysis (ABGA) revealed a pH of 7.07, PaCO2 of 22.4 mmHg, PaO2 of 123.7 mmHg, HCO3− of 6.4 mM/L, carboxy hemoglobin of 42%, and an O2 saturation level of 97% (mask ventilation with oxygen at 15 L/min). She was intubated prophylactically and transferred to the intensive care unit (ICU) for conservative treatment. The day after ICU admission, she showed a near-alert mental state but complained of dyspnea and chest discomfort. Her breath sounds included coarse wheezing and rhonchi. Chest plain radiography revealed peribronchial consolidations in both lungs. During ICU care, airway suction through the endotracheal tube was frequently performed, and her vital signs were stable. However, 5 days after ICU admission, she showed sudden tachypnea and tachycardia. At that time, her vital signs were as follows: blood pressure (BP), 192/111 mmHg; heart rate (HR), 125 beats/min; and respiratory rate (RR), 22 breaths/min. ABGA revealed a pH of 7.10, PaCO2 of 118.5 mmHg, PaO2 of 125.2 mmHg, HCO3− of 36.3 mM/L, and an O2 saturation level of 97% (mask ventilation with oxygen at 15 L/min). Six minutes after the onset of tachycardia, the patient appeared confused, and fingertip pulse oximetry revealed an O2 saturation level of 56%. Manual self-inflating bag-mask ventilation was performed to supply oxygen to the patient, but the physician in charge observed high airway pressure via the self-inflating bag mask. The patient’s BP decreased to 76/52 mmHg. We examined the endotracheal tube by using a fiberoptic bronchoscope and found that foreign bodies had almost completely blocked the lumen of the endobronchial tube tip. Removing the foreign bodies was difficult at that time, and the patient’s condition progressively worsened because of respiratory acidosis. Therefore, we decided to perform a tracheostomy instead of changing the endotracheal tube for resolving the airway obstruction. The foreign bodies removed through the tracheostoma were sloughed endobronchial debris, which might have obstructed the endotracheal tube (Fig. 1). After the removal of the sloughed endobronchial debris through the tracheostoma, the patient’s vital signs were as follows: BP, 127/78 mmHg; HR, 134 beats/min; and RR, 34 breaths/min. ABGA revealed a pH of 7.40, PaCO2 of 76.9 mmHg, PaO2 of 112.2 mmHg, HCO3− of 47.1 mM/L, and O2 saturation level of 98% (mask ventilation with oxygen at 15 L/min). We assessed the tracheobronchial condition by using a fiberoptic bronchoscope because her breath sounds included coarse wheezing. The bronchoscopy revealed that some debris remained in the tracheal lumen, nearly obstructing it. Chest computed tomography (CT) was used to evaluate the bronchiole. Chest CT revealed that 70% of the airway lumen was obstructed with debris at the level of the carina (Fig. 2). To restore airway patency, we decided to remove the endobronchial debris under general anesthesia in the operating room. General anesthesia with total intravenous anesthesia (TIVA) was considered because sudden movement of the patient or airway reaction could cause foreign bodies to move deeper into the bronchus during manipulation of the rigid bronchoscope. ECMO use rather than high frequency jet ventilation was decided during the operation because prolonged manipulation of the bronchoscope without ventilation could lead to hypoxia. The target concentration of propofol at the effect site was 2–2.5 μg/ml, and the target concentration of remifentanil was 3.5–4.5 ng/ml during general anesthesia with TIVA. Rocuronium (0.6 mg/kg) was administrated for facilitating rigid bronchoscopic manipulation. Systolic blood pressure was maintained between 100 and 120 mmHg; and diastolic blood pressure, between 50 and 75 mmHg during the intraoperative period. Heart rate was recorded between 65 to 90 beats/min. Oxygen saturation was maintained at 100% throughout the operation. Mechanical ventilation was intermittently applied with a tidal volume of 500 ml and at 12 breaths/min when ECMO was not applied. ECMO was applied for approximately 1 hour, and the venovenous approach through both femoral veins was used. Four pieces of foreign body were extracted by using rigid bronchoscopy. The total anesthesia time was 3 hours 20 minutes. The total operation time was 2 hours 40 minutes. The sizes of the foreign bodies were 7 × 3 cm, 3 × 2 cm, 1 × 0.5 cm, and 0.3 × 0.2 cm (Fig. 3). Bronchoscopy revealed no bleeding, but dark ash was stacked in both the main bronchus and carina (Fig. 4). Spontaneous respiration recovered within a few minutes after the administration of sugammadex (4 mg/kg). The patient was transferred to the ICU. ABGA revealed a pH of 7.45, PaCO2 of 35.0 mmHg, PaO2 of 113.6 mmHg, HCO3− of 24.0 mM/L, and O2 saturation level of 99% (FIO2 0.5) when she was admitted to the ICU. The following day, the endobronchial tube was removed. On hospital day 24, we confirmed by using bronchoscopy that her bronchus and carina were almost back to their original states (Fig. 5). She was discharged on hospital day 42, and her outpatient treatment is pending.
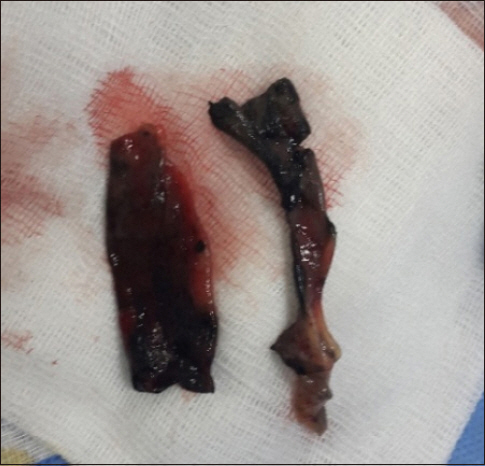
Removed foreign bodies (two pieces of endobronchial debris), which were suspected to obstruct the endotracheal tube, through the opening of the tracheostomy using fiberoptic bronchoscopy.

The lining of the airway was dissected up to the carina level, which was observed as a true/false lumen-like aortic dissection. The chest computed tomography scan shows definite evidence of upper airway obstruction at the level of the carina (white arrow).

Four pieces of foreign bodies at a deeper level of the bronchus that were removed under general anesthesia with total intravenous anesthesia and extracorporeal membrane oxygenation (ECMO). The sizes of the foreign bodies were 7 × 3 cm, 3 × 2 cm, 1 × 0.5 cm, and 0.3 × 0.2 cm.

The bronchoscopy image shows the lesions in the main bronchus and carina immediately after removing debris. No bleeding and dark ashes are stacked.
DISCUSSION
Inhalation burn injury can cause airway damage. High- temperature or chemical burns caused by the particulate constituents of smoke can be the causes of the injury. Inhalation burn injury can influence the survival of patients. Previous studies reported widely varying mortality rates. Edelman et al. [3] reported that patients with an inhalation injury had an overall mortality of 15%. Luo et al. [4] reported that the morbidity in patients with inhalation burns was 8.7%. The mortality and morbidity of patients with burn injuries depend on the severity of the inhalation burn injury. Upper airway injuries include direct thermal injury to the mouth, larynx, and oropharynx. These upper airway injuries can lead to upper airway obstruction during the first 12 hours [5]. Acute upper airway obstruction caused by laryngeal edema is the most crucial complication of inhalation burn injury and can lead to death. The larynx is the narrowest part of the upper airway and has a larger heat-retention capacity than the trachea. These properties of the larynx increase the risk of laryngeal edema, which can cause upper airway obstruction in patients with inhalation burn injuries. Orotracheal intubation is often impossible after complete airway obstruction by a laryngeal edema. Prophylactic intubation or tracheostomy should be considered before complete upper airway obstruction occurs [6]. Bronchospasm, pulmonary edema, bronchopneumonia, and lower airway obstruction are also airway complications of inhalation burn injury. The chemical components present in smoke can be toxins, which can lead to necrotic changes in the distal mucosal tissue. The airway mucosa of a healthy individual secretes mucus to eliminate foreign bodies. This is known as the mucociliary clearance mechanism [7]. However, the mucociliary clearance mechanism cannot function properly in patients with an inhalation burn injury because of mucosal damage. Therefore, these patients exhibit mucosal sloughing and develop a fibrinous exudate [8]. Examination of the airway patency by using bronchoscopy is important because lower airway obstruction can be caused by these sloughed endobronchial tissue debris and fibrin clots at deeper levels within a few days after the injury. Tracheostomy can be considered in patients who have no intact mucociliary clearance mechanism. Earlier tracheostomy may be necessary to facilitate pulmonary toilet of the obstructing clots and endobronchial debris in patients with severe inhalation injures [9,10]. In our patient, whose airway had started being obstructed by sloughed tissue debris, tracheostomy was a life-saving technique. Airway suction through the endotracheal tube or tracheostomy site, humidification of inspired air, and antibiotics for pulmonary infection may be helpful in such situations. However, prophylactic antibiotics or steroids bring no benefits [11]. In our case, the endobronchial debris was removed directly by using a rigid bronchoscope.
In case of airway obstruction, emergency tracheostomy or cricothyroidotomy may be considered for lifesaving. However, they can provide only limited effect depending on the level of obstruction. If in case of partial airway obstruction, pharmacological interventions such as corticosteroids, epinephrine, or inhaled heliox (a breathing gas composed of a mixture of helium and oxygen) may be temporarily helpful. However, it will be ineffective in mechanical upper airway obstruction. High-frequency jet ventilation is known as one of the most useful methods for such a case. However, we did not use it in the present case for the following reasons: It only works in the absence of complete airway obstruction. Furthermore, it can cause carbon dioxide retention and pneumothorax or pneumomediastinum. It can also cause foreign bodies to move deeper into the bronchus because of the high-pressure jet flow.
ECMO is an extracorporeal technique for restoring the cardiac and respiratory function of patients whose heart and lungs cannot provide adequate gas exchange to maintain life. Although ECMO was originally designed to support cardiac surgery, several reports have revealed that ECMO use can be a successful salvage maneuver in cases of lower airway obstruction [12,13]. ECMO provides sufficient gas exchange until airway patency is restored [14]. Therefore, the application of ECMO with TIVA was a good choice in our case because prolonged manipulation of the rigid bronchoscope without adequate ventilation could lead to hypoxia.
Compared with the conventional methods (i.e., intermittent ventilation and high frequency jet ventilation), ECMO can contribute to the safety of the patient. ECMO can facilitate the procedure by allowing the bronchoscopist or surgeon to focus on removing the tracheal obstruction regardless of a prolonged procedural time. Hence, the satisfaction of the surgeon was higher for the present procedure than for the conventional method of ventilation used in previous experiences. During the operation, the vital signs showed stable values and full oxygen saturation was well maintained. ABGA revealed normal tissue oxygenation. No postoperative airway complications occurred.
However, introduction of ECMO can lead to complications related to the procedure itself and its maintenance. Thus, it is important to manage the vascular complications. Common complications of ECMO include bleeding, thromboembolism, vascular injury from cannulation, and ischemia of the limb distal to an arterial cannula. ECMO specialists or perfusionists should perform careful visual inspection of the cannulae, ECMO circuit, and oxygenator for clots. It is necessary to evaluate hematocrit and platelet count frequently. Bedside monitoring of anticoagulation such as the activated clotting time for guidance of heparin dosing is also necessary. Fortunately, the patient in this case did not have any complications associated with ECMO. We regret not having conducted bispectral index monitoring in this case. During TIVA induction, the volume of distribution of the PK-PD model used in the target-controlled infusion device may be changed during ECMO, which may cause a difference between the actual blood/effect site concentration of the patient and the calculated concentration of the blood/effect site. Therefore, it is advisable to monitor the depth of sedation to avoid the risk of intraoperative recall.
This case provides a valuable experience and helped us suggest a successful anesthetic technique for managing acute lower airway obstruction. It is important to remember that sudden and unpredictable airway obstruction can be caused by sloughed endobronchial tissue debris in patients with inhalation burn injuries. Therefore, we recommend checking the airway patency frequently by using fiberoptic bronchoscopy whenever suspicions arise. Moreover, considering an alternative ventilation method such as tracheostomy or ECMO is highly important for cases in which complete airway obstruction is not only possible but also anticipated.