The sniffing position facilitated easier light wand guided endotracheal intubation compared with the neutral position with chin-lift
Article information
Abstract
Background
Traditionally, the patient's head is placed in a neutral position with a chin-lift to facilitate light wand guided endotracheal intubation. However, our study found that the sniffing position was more effective. In this study, we aimed to compare the two positions of light wand guided endotracheal intubation.
Methods
Sixty adult patients were included in the study, after obtaining informed consent, and were randomly assigned to one of two groups: a control group in a neutral position with a chin-lift (group C, n = 30) and a sniffing position group (group S, n = 30). In group C, the anesthesiologist inserted a light wand after lifting the patient's mandible using the thumb of their non-dominant hand inside the patient's mouth. In group S, a light wand was inserted after the patient's head was flexed with the neck extended. We assessed variables such as light-search time, number of intubation attempts, time to achieve intubation, and side effects including blood tinge on the endotracheal tube, hoarseness, sore throat, and anesthesiologist satisfaction.
Results
The light-search and intubation times were shorter in group S than in group C. The incidence of blood tinge on the endotracheal tube was higher in group C than in group S. Anesthesiologist satisfaction was higher in group S than in group C.
Conclusions
The sniffing position was more effective in facilitating light wand guided endotracheal intubation than the neutral position with a chin-lift.
INTRODUCTION
Light wands are primarily used in patients with difficult airways, such as those with restricted neck movement, limited mouth opening, or cervical spine disorders [1-3]. It can prevent damage to the teeth during intubation in patients with loose teeth by avoiding direct contact between the teeth and laryngoscope blade.
Previous clinical studies on intubation with a light wand positioned the patient’s neck in a neutral or slightly extended neck position with chin-lift [4-6].
When using the chin-lift method in a neutral position, the anesthesiologist’s non-dominant hand is positioned with the thumb in the molar area of the patient’s mouth and the rest of the fingers at the mandibular angle, while the dominant hand holds the light wand and inserts the endotracheal tube into the trachea. This method can be a safe option for minimizing cervical vertebral movement and can provide more space for the insertion of a light wand in obese patients or those with difficulty opening their mouths. However, this method has several limitations: the doctor’s thumb is contaminated, and there is a risk of further tooth damage in patients with loose teeth.
Based on our own clinical experience, we decided to place the patient’s head in the sniffing position. This alternative approach proved to be simpler and more efficient, with a successful insertion rate comparable to the neutral chin-lift position. Interestingly, our idea aligned with the suggestion made by Graham [7], who recommended the use of a lighted stylet as an excellent option for intubation in elective surgeries and difficult intubation cases. After years of experience with lighted stylets, they advocated their use as an alternative to direct laryngoscopy for intubation. Additionally, they taught their students to adopt the “sniffing” position, similar to the one used for laryngoscopy. They inserted the endotracheal tube into the right corner of the patient’s mouth and moved the tongue to the left, thereby eliminating the need for the physician’s hand to be placed inside the patient’s mouth.
The sniffing position consists of neck flexion and head extension, aligning the mouth and pharynx in a straight line and creating a natural oropharyngeal space, where a light wand can be inserted without the need for a chin-lift. This method may be inappropriate for patients who need to restrict their neck movement, but it is simple to perform as it does not require a chin-lift and is safe as there is no risk of touching the patient’s teeth.
While there have been recommendations on appropriate head positioning during light wand guided endotracheal intubation, few studies [8,9] have been performed to compare the efficacy of different head positions on the rate of successful insertion. Therefore, we compared the efficiency of two different head positions for light wand guided endotracheal intubation in patients without restrictions on neck movement or chin lifts.
We hypothesized that the sniffing position maneuver would better facilitate light wand guided intubation compared to the neutral position with a chin-lift. To test this, we compared the two positions for light wand guided intubation based on the primary variables of light-search time and intubation time as well as the secondary variables of postoperative sore throat and blood tinge.
MATERIALS AND METHODS
This clinical study was approved by the Institutional Review Board (Approval number H-1705-078-001) of the researcher’s affiliated hospital, and signed consent forms were obtained from all participants. This study was registered with the Clinical Research Information Service (Trial Registration number: KCT0005221) and conducted from August 2020 to August 2021.
This study enrolled adult patients scheduled for elective surgery who required tracheal intubation for general anesthesia. Eligible patients were between 18 and 80 years of age, with an American Society of Anesthesiologists physical status of 1-2 and who provided informed consent to participate in the study.
Exclusion criteria were: anatomical abnormalities in the neck, larynx, or pharynx, a body mass index ≥ 30 kg/m², or being at risk of aspiration. Patients with an expected intubation duration of less than 1 h or greater than 6 h or those unable to answer questions clearly were also excluded. Mouth opening and thyromental distance were measured in centimeters, and the modified Mallampati class was evaluated in patients before the start of anesthesia.
After entering the operating room, patients were monitored using electrocardiography, peripheral oxygen saturation, and noninvasive blood pressure measurements. General anesthesia was induced using 2 mg/kg propofol, the targeted effect-site of remifentanil was set at a dosage of 1-3 ng/ml, and rocuronium at a dosage of 0.6 mg/kg. Sevoflurane or desflurane was used to maintain anesthesia.
The patients were randomly assigned to one of two groups: the control group, which received intubation in the neutral position with a chin-lift, and the experimental group, which underwent intubation in the sniffing position. Assignment was determined using a computer-generated randomization table (http://www.randomizer.org).
Light wand (LightWandTM, GE Healthcare) guided endotracheal intubation was performed after verifying that the train-of-four (TOF-Watch SX®) count was zero following injection of the neuromuscular blocker.
One of the two experienced anesthesiologists skilled in using light wand guided endotracheal intubation performed the procedure. They were unaware of the patients’ modified Mallampati classification.
In the control group, a pillow was placed under the patient’s head to maintain a neutral position. To facilitate access of the light wand to the intraoral space, the anesthesiologist placed the thumb of their non-dominant near the patient’s molar teeth, while the remaining fingers held the mandible, lifting the patient’s jaw in the antero-caudal direction (Fig. 1).

To achieve the neutral position with chin-lift, an 8 cm pillow is placed under the patient’s head. The anesthesiologist positions their non-dominant hand’s thumb near the patient’s molar teeth while their remaining four fingers hold the mandible angle, lifting the jaw in an antero-caudal direction. The anesthesiologist’s dominant hand is used to hold the light wand.
In the sitting position group, a pillow was placed under the patient’s head to create neck flexion while the patient’s head was extended at the atlanto-occipital joint to promote head extension (Fig. 2). In both groups, the patients’ heads were positioned on the same pillow, 8 cm in height.

In the sniffing position group, a pillow measuring 8 cm in height was positioned under the patient’s head to induce neck flexion, while the anesthesiologist extended the patient’s head at the atlanto-occipital joint using their non-dominant hand. This posture naturally opens the patient’s mouth. The anesthesiologist holds the light wand with their dominant hand.
The end of the light wand was bent to 90°[5,9] at a point 8.5 cm from the end of the endotracheal tube (above the cuff) without forming a J-shape in both group, as the preparation itself is simple. The nurse, who did not know about the study, performed all bending; therefore, there was no difference in the shape of the tube tip between the two groups. Cuffed endotracheal tubes (ShileyMTM) were used, with dimensions of 7.5 mm and 6.5 mm for males and females, respectively.
In this study, we examined only the effect of the two head positions on intubation; thus we ensured that all remaining conditions, such as the bending angle, bending point from the tip, and pillow height, were consistent between the two groups.
During light wand guided intubation, the anesthesiologist used their dominant hand to hold the light wand in a manner similar to holding a pencil. The light wand was inserted into the right side of the patient’s oral cavity and moved toward the central line of the airway to enter the larynx. As the light wand moved through the airway, the anesthesiologist monitored the progress and looked for a bright light visible from the front of the neck down to the thyroid cartilage, indicating that the larynx had been intubated. Then light was removed from the mouth and the endotracheal tube was simultaneously advanced into the lower part of the airway. The success of intubation was confirmed by measuring the end-tidal carbon dioxide, which followed a normal pattern if the tube was correctly placed into the trachea.
In cases where light wand guided intubation failed twice, a direct laryngoscope was used as backup. If the peripheral oxygen saturation decreased below 100% during light wand guided intubation, the patient was ventilated using a face mask. The time taken to find the light below the area of the thyroid cartilage for each trial, endotracheal intubation time, anesthesia time, and operation time were recorded. Any side effects, including aspiration, regurgitation, hypoxia (SpO2 < 95%), bronchial spasm, mucosal or dental injury, and blood tinged on the endotracheal tube or in the oropharyngeal area that occurred during intubation or immediately after extubation, were recorded. During anesthesia, the intracuff pressure of the endotracheal tube was monitored every 30 min using a handheld aneroid manometer (VBMTM) and adjusted to maintain a pressure of 25 cmH2O. Hoarseness and sore throat (rated on a scale of 0-100) were recorded in the recovery room 30 min after the operation. The use of patient-controlled analgesia or additional analgesics during the recovery period were also documented.
The anesthesiologist who performed endotracheal intubation was aware of the patient's group allocation, while the assistant, who was unaware of the study, recorded the measured variables.
The light-search time was defined as the duration between the insertion of the light wand into the patient's mouth and the point of transillumination over the cricothyroid membrane. A maximum of two trials were allowed, with a time limit of 25 s for each attempt, after which the patient was ventilated with 2-5 vol% sevoflurane (100% oxygen) for 1 min.
Intubation time was defined as the duration from positioning the patient's head to the visualization of a normal pattern of end-tidal carbon dioxide. Intubation time was measured for the first and second attempts.
The degree of anesthesiologist satisfaction was evaluated after the patient was transferred from the post-anesthesia recovery room to the ward. The satisfaction levels were:1 = very unsatisfied, 2 = unsatisfied, 3 = satisfied, 4 = very satisfied, and 5 = extremely satisfied.
Statistical analysis
The sample size was calculated based on our pilot study, which had 10 patients per group; the mean difference in intubation time between the two groups was 10.7 s and the common standard deviation was 9.7 s. With an allocation ratio of 1:1, the required sample size was 28 per group, with an alpha error of 0.05, a beta error of 0.1, and a compliance of 0.8.
Continuous variables were expressed as mean (standard deviation), whereas categorical variables were presented as absolute values. Continuous variables including height and thyromental distance were compared using two-sample t-tests. Age, body weight, mouth opening, and anesthesia data were analyzed using the Mann-Whitney U test following the normality test. Categorical variables were compared using the chi-square test (sex and side effects) or– the Whitney test (American Society of Anesthesiologists, modified Mallampati class, trial frequency, and satisfaction).
A P value of < 0.05 was considered significant. All statistical analyses were performed using SPSS for Windows 27.0 (IBM Co.).
RESULTS
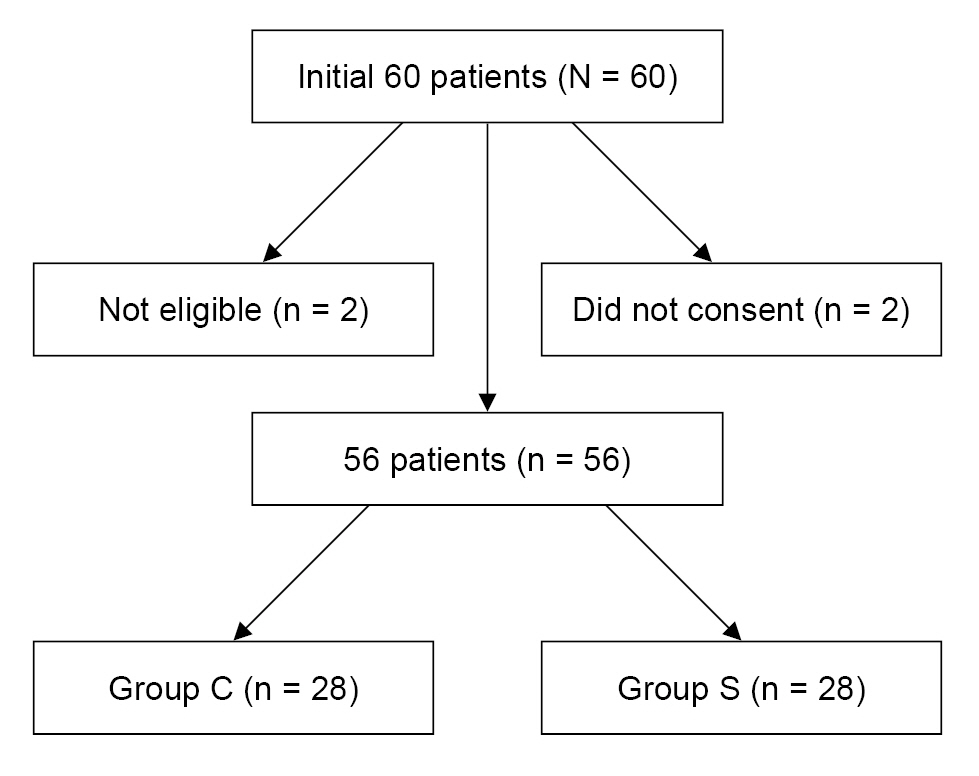
Initially, 60 patients were enrolled, 2 of whom did not consent to participate and 2 of whom were not eligible. The remaining 56 patients were included in the study and randomized (Fig. 3). All patients completed the study, and their data were analyzed. The patient demographic data are summarized in Table 1.
Light-search and intubation time were significantly shorter in the sniffing position group compared to the control group (8.4 ± 6.2 vs. 19.1 ± 17.0; P = 0.003, 29.3 ± 8.4 vs. 40.7 ± 17.1; P = 0.003, respectively) (Table 2).
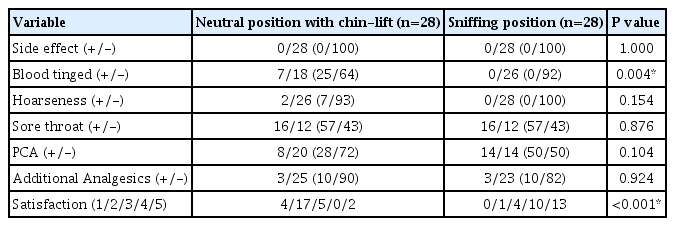
The incidence of blood tinge on the endotracheal tube or in the oropharyngeal area was higher in the control group than that in the sniffing position group (28% vs. 0%, P = 0.004) (Table 3).
Anesthesiologist satisfaction was significantly higher in the sniffing position than in the control group (4/17/5/0/2 vs. 0/1/4/10/13, P < 0.001) (Table 3).
DISCUSSION
Endotracheal intubation using a direct laryngoscope is the most widely used method for general anesthesia. However, this method requires a direct view of the larynx, and about 1-3% of the general surgical population experiences difficult or even impossible endotracheal intubation [10]. Consequently, alternative technologies have been developed over the years to prepare for difficult endotracheal intubations using a direct laryngoscope [10,11]. Light-guided endotracheal intubation is a coping technique that utilizes transillumination to safely and effectively guide the endotracheal tube into the airway without direct visualization of the larynx.
In a review article by David et al. [3], the use of the lighted stylet for tracheal intubation was discussed. They analyzed 10 studies that compared the lighted stylet technique with traditional methods of tracheal intubation. The results showed that, at the very least, the technique was comparable to traditional laryngoscopy. However, when utilized by skilled practitioners, it proved to be faster, more reliable, and better tolerated by patients. Furthermore, the use of an appropriate stylet allowed for its application in patients of all sizes without significantly increasing department costs. The authors recommended the implementation of this technique in all anesthetic departments and its inclusion in the training curriculum for medical trainees.
Light wands have typically been used in cases where direct laryngoscope-based endotracheal intubation is challenging or impossible, such as patients with limited mandibular protrusion, short thyromental distance, large neck circumference, high Mallampati grade airways, cervical injuries that limit neck movement, or those with unstable teeth that require avoidance of direct contact with laryngoscope blades during intubation [2,12,13].
The chin-lift method, in which the patient’s head is placed in a neutral position and the chin is lifted by an anesthesiologist, is commonly used for light wand guided endotracheal intubation [5,6]. To perform tracheal intubation, the thumb of the anesthesiologist’s non-dominant hand was placed inside the patient's mouth to lift the chin upward and secure the oropharyngeal space for light wand insertion. The anesthesiologist held the light wand in the dominant hand, inserted it into the right side of the oral cavity, and advanced it into the trachea alongside the endotracheal tube. However, this method may not be suitable for patients with shaky teeth as the teeth may be pulled out, and it may also lead to contamination of the anesthesiologist’s thumb with the patient’s saliva.
Upon discovering that lifting the jaw to its neutral position could potentially harm older patients with unstable teeth, the authors switched to the sniffing position for direct laryngoscope-based endotracheal intubation. The sniffing position, which involves placing a pillow under the patient’s head to flex the neck and extend the head to the atlanto-occipital joint, is commonly used for direct laryngoscope-based endotracheal intubation.
Suh et al. [9] compared the sniffing and neutral positions for light and intubation. A light wand railroad with an endotracheal tube was bent 90°, 5 cm from the distal end in both groups. The heads of the patients in the neutral position group were not placed on the pillow, whereas those in the sniffing position group used a 7 cm height pillow. They reported no significant differences in time to intubation, success rate, intubation time of the first trial, hydrodynamic changes, or BIS values between the two positions. The difference in pillow height between the study by Suh et al. [9] and our study would make the degree of neck flexion different; as a result, the angle between the oral and pharyngeal axes and the degree of mouth opening are different from those of our study. Their bending point was 5 cm from the end of the tube, which is also shorter than in our study (8.5 cm). In our study, two anesthesiologists performed the intubation, while Suh et al. [9] did not specify the number of researchers that performed the procedure. Therefore, it can be assumed that these differences in methods caused the differences between the study by Suh et al. [9] and ours.
Byun et al. [8] compared the success rates of light wand-facilitated tracheal intubation in the neutral and sniffing positions in 60 adult patients. The light wand and tube were bent at a 90° angle for the neutral group and at a 60° angle for the sniffing group based on the mouth and pharyngeal axes. The pillow height for both groups was 8 cm, which is with the same as in our study. There were no significant differences in the time to intubation, success rates of the first intubation trial, overall intubation success rates, hemodynamic changes, or complications between the two positions. Our study followed a method similar to that used by Byun et al. [8], except for the angle at which the end of the tube was bent in the sniffing group. However, despite this difference, our results differed significantly from those of Byun et al. [8], indicating that factors such as the angle between the oral and pharyngeal axes in the sniffing group and the bending point of the tube likely influenced the outcomes.
As anticipated, the success rates of the two groups in our study did not differ. The head position itself is unlikely to significantly affect the success rate, as anesthesiologists strive to quickly achieve airway patency and overcome obstacles [14]. This viewpoint is supported by the fact that the anesthesiologists in the sniffing position group reported higher satisfaction scores than those in the neutral position group in our study.
Placing the patient's head in a sniffing position naturally opens the mouth and creates space for the light wand to pass without lifting the chin. This position also straightens the anterior neck, which may make light more visible during intubation [15].
The extent of tube bending, location of the bending point from the end of the tube, use of a pillow, position of the patient’s head, and specific clinical conditions (such as the involvement of multiple anesthesiologists) differed between our study and previous ones [8,9]. These variations likely contributed to the difference between their results and ours.
This study has several limitations. First, we excluded patients with anatomical airway abnormalities or body mass index ≥ 30 kg/m², so it may be difficult to apply our results to patients with those characteristics. Additionally, because our patients had lower modified Mallampati scores, it is unclear how well our findings would apply to patients with higher scores.
Second, the anesthesiologist performing endotracheal intubation could not be blinded to the patient grouping; thus, they refrained from participating in the assessment of variables to minimize potential bias. However, some bias may still exist owing to the single-blind method used in the study.
For patients with cervical mobility restrictions, the neutral position should be used with the chin-lift method instead of the sniffing position during light wand guided endotracheal intubation.
However, in this clinical study, the sniffing position was found to be more effective in facilitating endotracheal intubation using a light wand than the neutral position with a chin-lift.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Mi Jung Yun. Data curation: Gunn Hee Kim. Formal analysis: Gunn Hee Kim, Mi Jung Yun. Methodology: Gunn Hee Kim, Mi Jung Yun. Project administration: Gunn Hee Kim, Eun Jae Jung, Yun Jae Han, Mi Jung Yun. Investigation: Eun Jae Jung, Yun Jae Han, Mi Jung Yun. Resources: Mi Jung Yun. Supervision: Mi Jung Yun. Validation: Gunn Hee Kim, Mi Jung Yun. Writing - original draft: Gunn Hee Kim. Writing - review & editing: Mi Jung Yun, Gunn Hee Kim.
Acknowledgements
We would like to thank all the surgical and operating room members of the Medical Center for their support in conducting this study.