 |
 |
- Search
| Anesth Pain Med > Volume 17(3); 2022 > Article |
|
Abstract
Background
Submental intubation has been the recommended airway management procedure for maxillofacial surgery since proposed by Altemir in 1986. We adopted various submental intubation modifications based on modified intubation protocols and report on the effectiveness and problems of each modified method.
Case
Among a total of 13 submental intubation cases during the last five years, five representative methods are described. The proximal end of the endotracheal tube was protected by a nelaton catheter in case 1, by a suction connector in case 2, and by a dental needle cap in case 3. In case 4, a nasal speculum was used to expand a single route, and in case 5, a laparoscopic trocar was used to secure a single route.
Anesthesiologists must make careful decisions about airway management in maxillofacial surgery. Although nasal intubation is preferred, it is not recommended in cases of midface injury or nasoethmoidal complex fracture where intracranial intubation is expected [1]. In these cases, tracheotomy is often performed, which is far from the surgical site and enables a stable and safe airway; however, tracheotomy is invasive and has a risk of multiple complications [2,3]. In 1986, Altemir [4] proposed submental intubation as an alternative to nasal intubation and tracheotomy. Submental intubation is much simpler, more convenient, and presents with a lower incidence of complications than tracheotomy [5]. Since Altemir first proposed the submental intubation method, several modified methods have been reported [6-10]. Here, we undertook a total of 13 submental intubation cases over the last five years during anesthesia in maxillofacial surgery (Table 1) and report five representative methods. We describe the problems associated with each modified method and present the most effective modification along with a literature review.
The current report was approved by Institutional Review Board (no. CR321147). Written informed consent to publish these cases was obtained from all patients. The patients underwent open reduction and internal fixation surgery for facial fractures, and a wire reinforced endotracheal tube (Covidien, Ireland) was used for intubation. Since this tube is glued so that the connector part is not separated from tube, the proximal end of the tube and the connector part were separated in advance before performing the procedure. When the patient was admitted to the operating room, pulse oximetry, electrocardiogram, and non-invasive blood pressure monitoring were initiated, and preoxygenation was performed on the patient through a facial mask for about 5 min. After induction with propofol, remifentanil, and rocuronium, oral intubation was performed using a video laryngoscope, and anesthesia was maintained with sevoflurane or desflurane. To create the submental route, a parallel incision was applied to the submental skin about 2 cm posterior to the inferior border of the mandible symphysis. The platysma muscle and mylohyoid muscle were bluntly dissected using a curved hemostat to prepare for passage into the oral cavity. After mouth opening with a retractor, the mouth floor was exposed by retracting the tongue laterally using an Army-Navy retractor. After applying a stab incision to the corresponding sublingual mucosa by palpating the hemostat tip with a finger and taking care not to damage the Warton’s duct on both sides, the hemostat was advanced to expose the tip into the oral cavity to secure a route for the tube to pass. Since ventilation was not available during the passage of the endotracheal tube through the submental route, sufficient preoxygenation was performed with 100% O2 before separation from the ventilator.
A 24-year-old male patient with a Le Fort II fracture, nasoethmoidal fracture, orbital wall fracture, mandible fracture, and basal skull fracture.
After submental tunnel formation and preoxygenation, the pilot balloon was passed through the submental route. After the endotracheal tube connector was disconnected, a nelaton catheter (Sewoon Medical Vina Co., Vietnam) was placed on the proximal end of the endotracheal tube (Fig. 1A). The distal end of the nelaton catheter was passed through the submental tunnel and the endotracheal tube was manually pushed through the secured route. Next, the nelaton catheter was removed from the endotracheal tube, and ventilation was resumed by connecting the connector and the endotracheal tube. After confirming that ventilation was normal, the skin of the submental region was sutured using black silk to fix the position of the tube.
A 19-year-old male patient with a pan-facial fracture.
After submental tunnel formation and preoxygenation, the pilot balloon was passed through the submental route. After the endotracheal tube connector was disconnected, a suction connector (Sewoon Medical Vina Co.) was connected to the proximal end of the endotracheal tube (Fig. 1B). After passing the hemostat through the submental route from the outside, the suction connector was caught in the oral cavity and passed outside. However, multiple routes were formed during the submental tunnel dissection process, and as a result, it was confirmed that the pilot balloon and endotracheal tube passed through different routes. After returning the endotracheal tube back to the intraoral space, the route through which the pilot balloon passed was secured, passed through the hemostat, and then the suction connector was held and passed. Next, the suction connector was removed from the endotracheal tube, and ventilation was resumed by connecting the connector and the endotracheal tube. After confirming that ventilation was normal, the skin of the submental region was sutured using black silk to fix the position of the tube.
A 39-year-old male patient with a pan-facial fracture.
In Case 2, the pilot balloon and endotracheal tube were passed through different submental routes, so the method proposed by Oshima et al. [10] was referenced to secure a single route. After the submental tunnel was made, black silk (Covidien) was passed through a secured single route (Fig. 1C). The black silk was pulled from the oral area after grabbing it with a hemostat from the submental area. Then, the hemostat was passed through the submental tunnel and the pilot balloon was held using the hemostat to pass it through the submental area. Next, the endotracheal tube connector was disconnected, and a dental needle cap (CK Dental Industries, Korea) was inserted into the proximal end of the endotracheal tube and then wrapped with Ioban (3M, USA) to prevent disconnection (Fig. 1D). After the hemostat was placed as in Case 2, the proximal end of the dental needle cap was grabbed and pulled out to the submental region. Next, the Ioban was removed, the dental needle cap was disconnected from the endotracheal tube, and ventilation was resumed by connecting the connector and the endotracheal tube. After confirming that ventilation was normal, the skin of the submental region was sutured using black silk to fix the position of the tube.
A 31-year-old male patient with pan-facial fracture accompanied by a frontal base traumatic subarachnoid hemorrhage.
Before passing the pilot balloon through the submental route, a nasal speculum was inserted into the submental tunnel from the outside to secure a single route and expand the tunnel (Fig. 1E). The pilot balloon was passed through the secured route. Next, the endotracheal tube connector was disconnected, and the hemostat was passed through the secured single route holding the proximal end of the endotracheal tube and passing it through. Ventilation was resumed by connecting the properly placed endotracheal tube, connector, and ventilator. After confirming that ventilation was normal, the skin of the submental region was sutured using black silk to fix the position of the tube.
A 23-year-old male patient with pan-facial fracture accompanied by a traumatic subdural hemorrhage.
To secure a single submental route and a separated tunnel, a laparoscopic trocar (Ethicon, USA) was used referring to the method proposed by Jung et al. [6]. After passing the laparoscopic trocar from the outside through the skin incision and mucosal incision, the puncture needle was separated to secure the route (Fig. 1F). After first passing the pilot balloon through the trocar route, the endotracheal tube connector was disconnected, and the proximal end of the endotracheal tube was pushed through the trocar route. Next, the trocar was removed, and ventilation was resumed by connecting the endotracheal tube, connector, and ventilator. After confirming that ventilation was normal, the skin of the submental region was sutured using black silk to fix the position of the tube.
In all cases, after open reduction and internal fixation were completed, the black silk suture fixing the endotracheal tube was removed to reposition the endotracheal tube to the intraoral position. The connector was separated, and the endotracheal tube was pulled from inside of the mouth so that the tube passed through the submental route to be repositioned intraorally. Then, the pilot balloon was repositioned into the oral cavity in the same way. Ventilation was resumed by reconnecting the connector and ventilator and the submental incision was sutured. In Case 3, the wire-reinforced endotracheal tube was exchanged for a conventional endotracheal tube for ventilator care in the intensive care unit (ICU). All other cases were extubated in the operating room, and all patients were transferred to the trauma ICU.
In maxillofacial surgery, nasal intubation, tracheotomy, and submental intubation are the suggested methods for securing an airway. Nasal intubation is relatively less invasive than other airway management procedures and has the advantage of being easy to perform; however, there is a risk of complications such as epistaxis, bacteremia, intranasal submucosal laceration, and intracranial intubation [11,12]. Tracheotomy does not invade the surgical site, but it is the most invasive technique. In addition, tracheotomy leaves visible scars and can lead to several complications such as esophageal injury, damage to major vessels and nerves of the neck, pneumothorax, and tracheal stricture [2,3].
Submental intubation avoids the fatal complications of nasal intubation and is less invasive and is easier to secure the airway than in tracheotomy [5]. In the method suggested by Altemir [4], normal oral intubation is first performed, and then the endotracheal tube is passed through a 2-cm paramedian incision tunnel that passes through the skin of the submental region and the mucosa of the lingual aspect mandible. After surgery, the endotracheal tube is repositioned to the oral position and the incision is completed with a suture. However, submental intubation can also cause various complications. There are complications resulting from the incision site, such as bleeding, infection, orocutaneous fistula, mucocele, and/or tube obstruction due to endotracheal tube damage, blood clots, or soft tissue [13,14].
In the several reported endotracheal intubation methods [6-10], a wire-reinforced endotracheal tube was used to prevent obstruction due to bending or damage of the endotracheal tube, which we used in all trials. Also, to prevent obstruction caused by the entry of foreign substances into the tube and complications due to route incision, we utilized various methods of submental intubation.
The method used in Case 1 (Patient 1) included covering the proximal end of the endotracheal tube with a nelaton catheter and then first passing the nelaton catheter through the submental route to pass the endotracheal tube through the submental route without damaging the surrounding tissue with minimal incision. An advantage of this method is that the endotracheal tube covered by the nelaton catheter prevents tube obstruction caused by blood clots or soft tissue. However, in the process of pulling the nelaton catheter from the outside of the mouth to pass the endotracheal tube through the submental route, the situation where the nelaton catheter was separated from the endotracheal tube was repeated several times. To prevent this, the nelaton catheter was pulled with enough force to not separate it from the endotracheal tube from the outside of the mouth, and the endotracheal tube was pushed in the mouth at the same time. During this process, it was difficult for the tube to easily pass through the submental incision site, and excessive pressure was required, which may accompany damage to the surrounding soft tissue. Due to concerns about the continuation of apnea due to frequent separation and excessive damage to the soft tissue during the passage of the submental route, we attempted a different method in Case 2.
In Case 2 (Patient 4), a suction connector was connected to the proximal end of the endotracheal tube. Compared to the nelaton catheter, it can be firmly inserted into the proximal end and has a smaller diameter than the tube such that it was possible to prevent entry of blood clots or soft tissue. Since the material of the suction connector is plastic, it was easy to hold using a hemostat when pulling the tube out of the mouth. However, there was a situation in which the suction connector was broken due to the pressure applied by the hemostat. If this fragment enters the tube, there is a risk that the tube obstruction or foreign body may enter the lung. In this case, two different routes were formed by the remnant soft tissue created by blunt dissection with the hemostat in the process of making the submental tunnel. There was a situation in which the pilot balloon and the endotracheal tube passed through the different routes formed by the remnant tissue. Therefore, it was necessary to attempt a different method to secure a single submental route and address the need for a material that does not break with hemostat use, as in Case 3.
In Case 3 (Patient 5), a dental needle cap was connected to the proximal end of the endotracheal tube. Unlike the suction connector, the dental needle cap is a material that does not break when held with a hemostat, and can completely block the tube without a lumen, so there is no risk of blood clots or soft tissue entering the tube. In addition, as a result of using the method of securing a single submental route using black silk proposed by Oshima et al. [10], the problem of forming two different routes by remnant soft tissue was solved. However, even with this method, when the endotracheal tube was pulled out of the submental incision site, it did not pass through smoothly, and excessive pressure was applied to the surrounding soft tissue.
In Case 4 (Patient 8), we focused on securing and expanding the submental route. After making the submental tunnel, the single expanded route was secured using a nasal speculum. By allowing the endotracheal tube to pass through the nasal speculum, unnecessary pressure was not transferred to the surrounding soft tissue when the tube was removed, and blood clot and remnant soft tissue issues that could cause tube obstruction did not occur.
In Case 5 (Patient 13), the submental route was secured using a laparoscopic trocar as presented by Jung et al. [6]. This method has the disadvantage of high cost, but the risk of obstruction of the endotracheal tube was significantly reduced because it was possible to secure a tunnel separated from the surrounding soft tissue more reliably than the nasal speculum. In addition, the trocar was relatively easy to use and was reliable.
We recognize that this case series has limitations as it is a retrospective review. In addition, the size of the case series is small. In particular, we could not measure the time needed to perform submental intubation in each case. Further comparative studies of trocar and nasal speculum are necessary.
In summary, the important points in submental intubation are securing a single submental route, preventing tube obstruction, preventing unnecessary soft tissue damage during tube passage, and minimizing apnea time. Judging from our experience, the laparoscopic trocar method is recommended as an easy and reliable way to secure a single submental route. However, since laparoscopic trocar use is costly, the nasal speculum method is also recommended based on cost-effectiveness.
Notes
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Hyun Kyo Lim. Data curation: Dongeui Hong, Yeong-gwan Jeon. Methodology: Yeong-gwan Jeon, Chunui Lee, Hyun Kyo Lim. Project administration: Yeong-gwan Jeon. Writing - original draft: Dongeui Hong. Writing - review & editing: Yeong-gwan Jeon, Hyun Kyo Lim. Investigation: Younghyun Jin. Resources: Chunui Lee. Supervision: Hyun Kyo Lim.
Fig. 1.
Various submental intubation modifications and instruments. The proximal end of the endotracheal tube was protected by a nelaton catheter in Case 1 (A), and by a suction connector in Case 2 (B). To secure single route, black silk was passed through a submental route in Case 3 (C). The proximal end of the endotracheal tube was protected by a dental needle cap in Case 3 (D). To secure a single route a nasal speculumt was used in Case 4 (E), and a laparoscopic trocar was used in Case 5 (F).
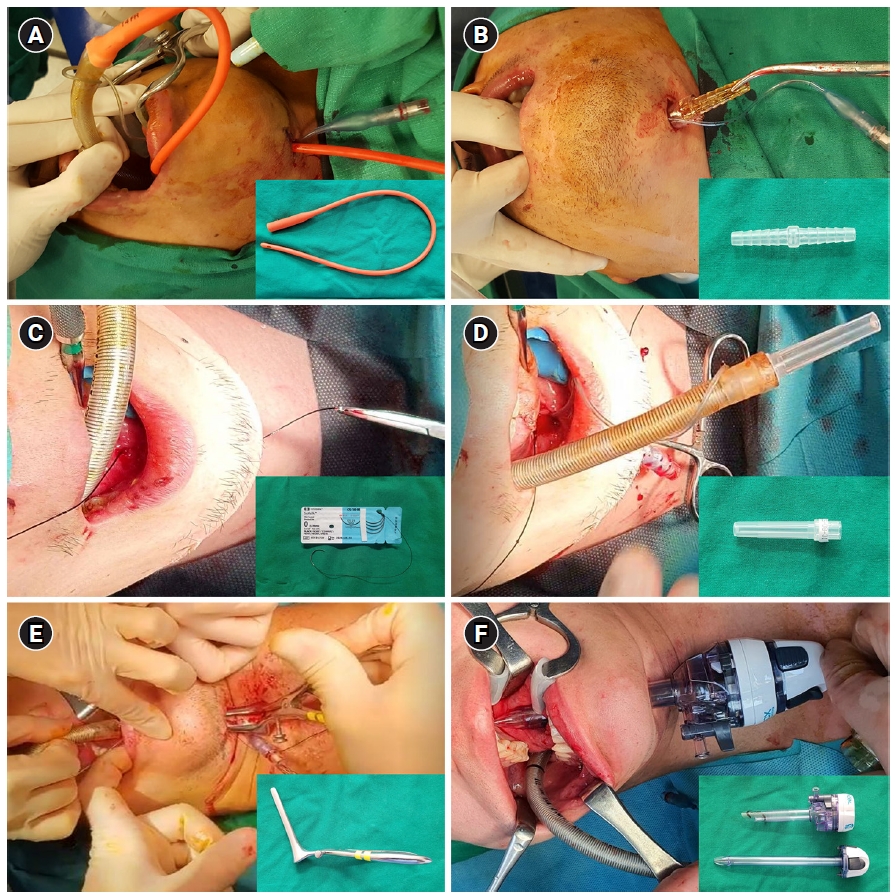
Table 1.
Thirteen Submental Intubation Cases during the Last Five Years
REFERENCES
1. Caubi AF, Vasconcelos BC, Vasconcellos RJ, de Morais HH, Rocha NS. Submental intubation in oral maxillofacial surgery: review of the literature and analysis of 13 cases. Med Oral Patol Oral Cir Bucal 2008; 13: E197-200.

2. Halum SL, Ting JY, Plowman EK, Belafsky PC, Harbarger CF, Postma GN, et al. A multi-institutional analysis of tracheotomy complications. Laryngoscope 2012; 122: 38-45.


3. Straetmans J, Schlöndorff G, Herzhoff G, Windfuhr JP, Kremer B. Complications of midline-open tracheotomy in adults. Laryngoscope 2010; 120: 84-92.



4. Hernández Altemir F. The submental route for endotracheal intubation. A new technique. J Maxillofac Surg 1986; 14: 64-5.

5. Caron G, Paquin R, Lessard MR, Trépanier CA, Landry PE. Submental endotracheal intubation: an alternative to tracheotomy in patients with midfacial and panfacial fractures. J Trauma 2000; 48: 235-40.


6. Jung I, Yoo BH, Ju JY, Choi S, Yon JH, Kim KM, et al. Novel alternative for submental intubation - a case report. Anesth Pain Med (Seoul) 2020; 15: 247-50.




7. Lim HK, Kim IK, Han JU, Kim TJ, Lee CS, Song JH, et al. Modified submental orotracheal intubation using the blue cap on the end of the thoracic catheter. Yonsei Med J 2003; 44: 919-22.


9. MacInnis E, Baig M. A modified submental approach for oral endotracheal intubation. Int J Oral Maxillofac Surg 1999; 28: 344-6.


10. Oshima N, Shiraishi T, Kawauchi T, Oba J, Sato D, Fujiki M, et al. A simple and reliable submental intubation technique for maxillofacial fractures. J Craniofac Surg 2018; 29: 1952-5.



11. Chen YH, Chen JY, Hsu CS, Huang CT, So E. Recurrent epistaxis following nasotracheal intubation--a case report. Acta Anaesthesiol Sin 1996; 34: 93-6. Erratum in: Acta Anaesthesiol Sin 1996; 34: 172.
12. Enk D, Palmes AM, Van Aken H, Westphal M. Nasotracheal intubation: a simple and effective technique to reduce nasopharyngeal trauma and tube contamination. Anesth Analg 2002; 95: 1432-6.


-
METRICS

-
- 2 Crossref
- 2,657 View
- 73 Download
- Related articles in Anesth Pain Med
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others







